Using Dentrix, you can post EOB claim payments or adjustments for one claim at a time or for all claims associated with an ERA, check, or credit card. You can also split a primary claim, edit a claim, apply a deductible, update the payment table, add a claim status note, enter and split an adjustment by provider, calculate provider balances, and generate a statement. To avoid the possibility of posting the same EOB multiple times, the claim is locked so that you cannot open it on more than one computer simultaneously. You can view the file on another computer, but you cannot make any changes to the claim.
To post a batch electronic insurance payment
1. In the Ledger, click File, and then click Enter Batch Ins. Payment.
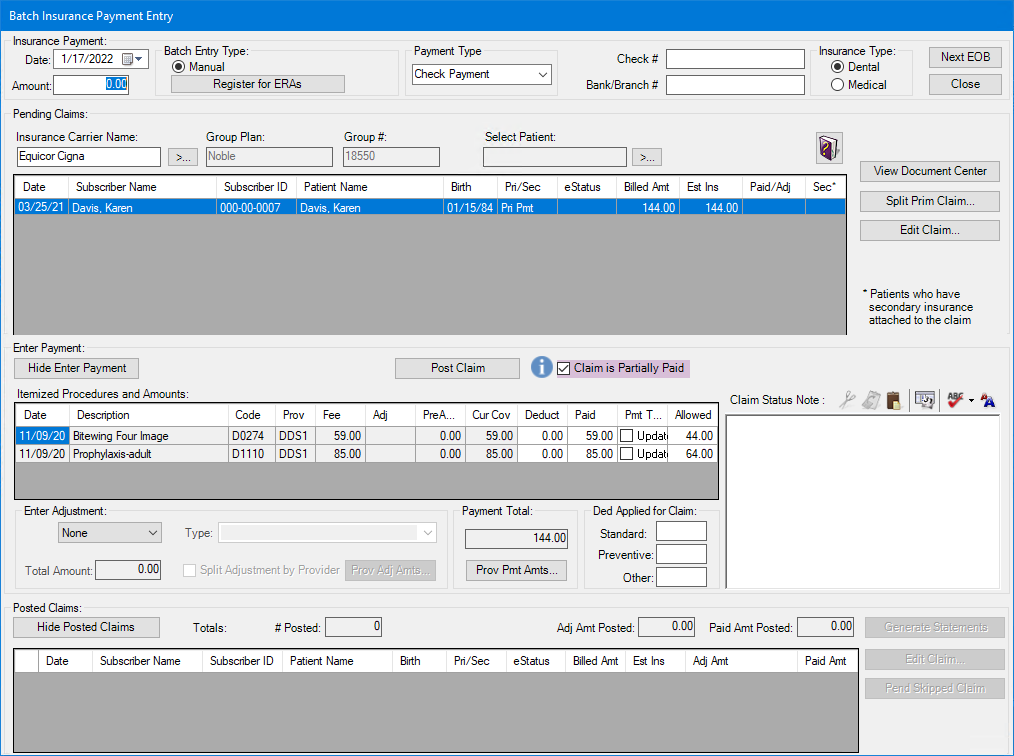
The Batch Insurance Payment Entry dialog box appears.
Notes:
The Payment Type, Check #, and Bank/Branch # fields are read from the ERA and fill in automatically.
Under Pending Claims, the Sec column indicates whether a patient's secondary insurance is attached to the claim. Under Enter Adjustment, the Information icon (blue circle with the letter i in white) also indicates that the patient has secondary insurance.
The Amount of field under Insurance Payment is also read from the ERA and fills in automatically. The Amount of field is hidden by default and is only made available by request to Dental Service Organizations (DSO). In the example above, the total payment received was $500, but that amount was split between two offices with the same Tax Identification Number ($320 to one and the remaining $180 to the other).
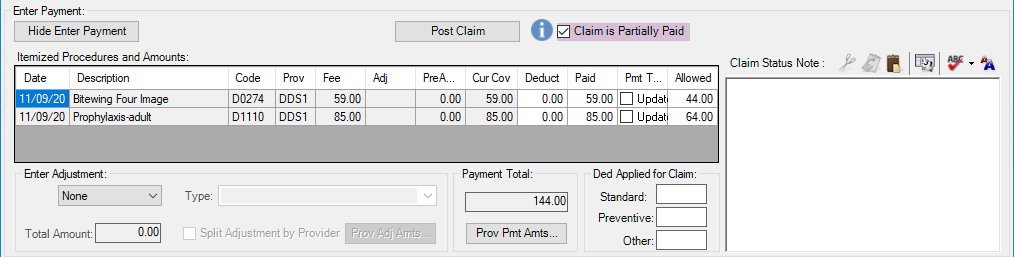
The Claim is Partially Paid check box indicates that a claim is partially paid and will not have a status of received. The flag can be changed when an insurance payment is added or edited. The flag can also be changed in the Insurance Claim Status dialog box.
2. Click the Select ERA search button.
The Select ERA dialog box appears.
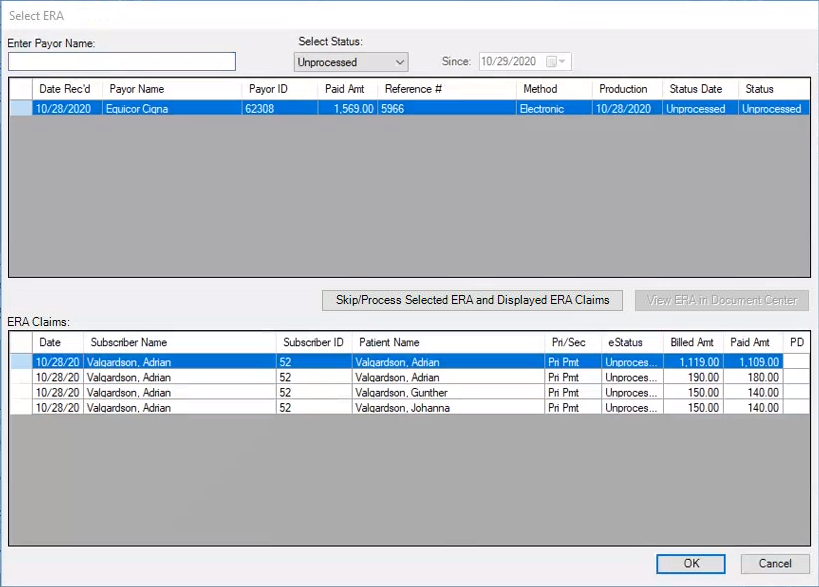
3. Type a payor’s name or select an ERA from the list, and then click OK.
The Batch Insurance Payment Entry - Electronic dialog box appears, and all EOB claims associated with the ERA appear in the Pending Claims list.
Note: If you receive an EOB claim payment for a Dentrix claim that has already been paid or received, you can post the payment as an additional payment to the "received" Dentrix claim, or you can select another Dentrix claim to apply the EOB claim payments or adjustments related to the Dentrix claim.
4. Select an EOB claim with an eStatus of OK - Post from the Pending Claims list.
The claim appears in the Itemized Procedures and Amounts list.
Note: If you receive an ERA for a claim that is not in the database, a message appears saying that the claim could not be found and from which you can select a different Dentrix claim to apply the ERA to or set the EOB claim to "skipped."
5. Under Enter Payment, click Post Claim to post the claim.
The claim appears in the Posted/Skipped Claims list.
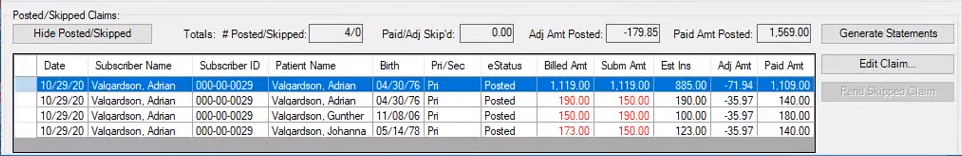
6. Under Posted/Skipped Claims, click Next EOB to process and post the next EOB, or click Generate Statements to generate a billing statement.