Changing claim details
You can change details of a primary claim that has not been paid: procedures, diagnosis (ICD-10) codes, billing and rendering providers, payer information, additional claim information, attachments, and status notes. Also, the patient and subscriber information appears for your reference.
Note: On secondary and tertiary claims, you cannot change all the details that you can for primary claims.
To change claim details
-
Click (or tap) a claim on one of the following pages:
-
How to get there
-
On the Home menu, under Insurance, click (or tap) Unsent Claims.
The Unsent Claims page opens.
The Unsent Claims page.

-
-
How to get there
-
On the Home menu, under Insurance, click (or tap) Sent Claims.
The Sent Claims page opens.
The Sent Claims page.

-
-
How to get there
-
If the correct patient is not already selected, use the Patient Search box to access the patient's record.
Note: You can include inactive patients in the search results by setting the Include inactive patients switch to On.
-
On the Patient menu, under Insurance, click (or tap) Insurance Claims.
The patient's Insurance Claims page opens.
A patient's Insurance Claims page.

-
-
How to get there
-
If the correct patient is not already selected, use the Patient Search box to access the patient's record.
Note: You can include inactive patients in the search results by setting the Include inactive patients switch to On.
-
Do one of the following:
-
On the Patient menu, under General, click (or tap) Overview. The patient's Overview page opens. Click (or tap) the Ledger box.

-
On the Patient menu, under Financial, click (or tap) Ledger.
The patient's Ledger page opens.
-

-
The Claim Detail dialog box appears.
Unsent Claim

Queued, Sent, Printed, Rejected, or Received Claim

-
-
Change the details as needed on any of the following tabs:
-
Procedures
The Procedures tab displays the associated procedures and conditions.

Modify the procedures on the claim as needed:
-
To add procedures procedures to the claim, click (or tap) Add Procedure. The Add Procedures dialog box appears and lists procedures that have the same date of service as the procedures already on the claim. Select the checkboxes of the procedures that you want to add, or select the checkbox in the column header to select all procedures. Then, click (or tap) Add Selected.

-
To remove procedures from the claim, select the checkboxes of the procedures that you want to remove, or select the checkbox in the column header to select all procedures. Then, click (or tap) Remove Selected. If you attempt to remove all procedures from the claim, a message appears and asks if you want to delete the claim and any associated payments and adjustments. Click (or tap) Delete to confirm the deletions.

Note: If an automatic write-off adjustment was posted for the claim, when you change the procedures, the adjustment is replaced or deleted as needed.
For the procedures on the claim, the associated diagnoses appear. You can have up to four ICD-10 codes per claim. Modify the diagnoses as needed:
-
To remove ICD-10 codes, click (or tap) the corresponding Remove buttons
 .
.
Note: Removing ICD-10 codes from a claim does not affect the corresponding procedures. All diagnoses remain attached to their corresponding procedures as currently posted in the patient's ledger and progress notes.
-
If you have less than four ICD-10 codes, to add an ICD-10 code to the claim, select a diagnosis from the Select a diagnosed condition list. Only the diagnoses attached to the claim's procedures (as currently posted in the patient's ledger) are available for selection. If there are two, three, or four ICD-10 codes, select the one that you want to be the primary diagnosis.

-
-
General
The General tab displays billing and rendering provider information, the pay-to address, patient information, subscriber information, and payer information.

Change the Billing Provider and/or Rendering Provider as needed. Only providers who have access to the location where the claim was created are available.
Also, if the selected Rendering Provider has been designated as a locum tenens treating provider in his or her user account, the Locum Tenens Treating Provider switch is set to Yes by default; otherwise, it is set to No by default. You can change the state of the switch if necessary; however, the locum tenens treating provider is not required for most claim form versions; currently, this setting affects only printed 2024 ADA claim forms, and the carrier's selected Printed claim format must be the 2024 version to include this information on printed claims.
Note: If the patient's insurance plan details have changed since the claim was created, a yellow warning symbol appears on the General tab, and next to Payer. Click the Refresh button
 to update the payer information.
to update the payer information.
-
Claim Info
The Claim Info tab displays the name of the referring provider, the reference number, orthodontia information, orthodontia information, remarks for unusual services, accident information, and the place of service.
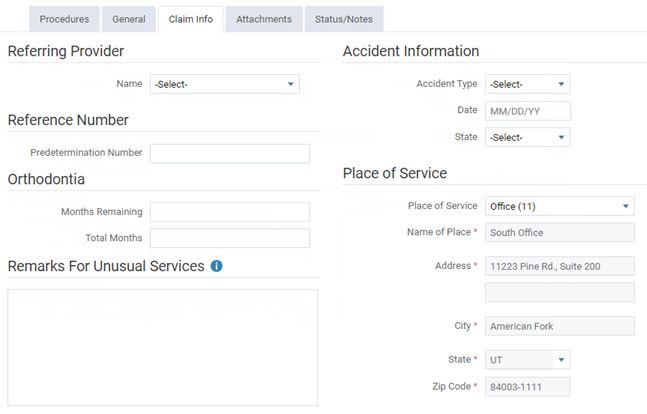
Enter or change any of the information as needed:
-
Referring Provider - Select a provider from the Name list.
-
Reference Number - In the Predetermination Number box, enter the predetermination (pre-authorization) reference number.
-
Orthodontia - If the claim was created for orthodontic treatment, enter orthodontia information. In the Months Remaining box, enter the number of months remaining. In the Total Months box, change the total number of months if applicable. The default value for Total Months is calculated automatically based on the placement date and remaining months specified.
-
Remarks for Unusual Services - Enter notes for the insurance carrier for this claim only.
Note: Only the first 80 characters are submitted electronically even though the box allows up to 151 characters.
-
Accident Information - Select the Accident Type, specify the Date, and select the State.
-
Place of Service - The default place of service for the claim is determined by the Place of Service Default Location on the Insurance Defaults page. The address fields are populated automatically with the address where the services were rendered (the location associated with the procedures on the claim).
You can select a different location type from the Place of Service list if applicable. Also, depending on the Place of Service Default Location, you may be able to change the Place of Service address for an individual claim:
-
If the Place of Service Default Location has been changed to a location type other than Office (11) since the claim was created, and if the claim's Place of Service is Office (11), the service location's name and address appear and cannot be edited.

-
If the Place of Service Default Location has been changed to a location type other than Office (11) since the claim was created, and if the claim’s Place of Service matches the Place of Service Default Location, the service location's name and address appear but can be edited.

-
If you change the Place of Service to a location type other than the Place of Service Default Location, you must specify the name and address of the service location.

-
If you change the Place of Service to a location type that is the same as the Place of Service Default Location, the service location's name and address appear and cannot be edited.

Notes:
-
For the place of service address, the following information is required: Name of Place, Address (the first box only), City, State, and Zip Code (ZIP Code + 4).
-
The place of service address appears on a printed claim only if the ADA claim form version is 2019 or 2024. The place of service address is transmitted with every electronic claim.
-
-
-
Attachments
The Attachments tab, displays the patient's images from Dentrix Ascend Imaging, images from the patient's document manager, the patient's perio exam, and the patient's clinical notes that are attached.
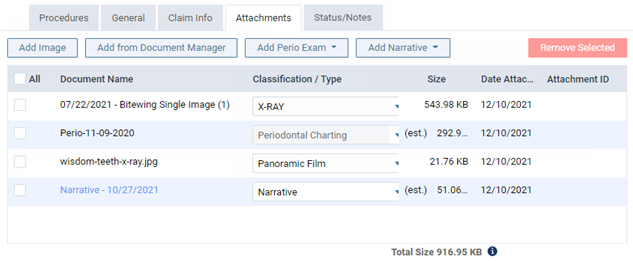
Note: To reduce delays or non-payments from insurance carriers, Dentrix Ascend alerts you when, according to NEA guidelines, supporting documentation is recommended for any procedures on a claim. An orange warning icon and a message with the applicable procedures and recommended attachment types appear when claim attachments are recommended. For a secondary (or tertiary or quaternary) insurance claim, a warning message includes a recommendation to attach the EOBs from the corresponding primary (and/or secondary and/or tertiary) claims before submitting the secondary (or tertiary or quaternary) claim.

You can ignore a warning and submit the claim without the recommended attachments.
Important: Ignore an attachment recommendation only if you are certain that the payer does not require supporting documentation for the procedure.
Add and remove attachments as needed:
-
To attach an image from Dentrix Ascend Imaging, click (or tap) Add Image. In the Add from Imaging dialog box, click (or tap) a procedure with the correct date of service to view the corresponding images. Select the checkbox next to the procedure name to attach all the images in that section to the claim, or individually select the checkboxes of images that you want to attach to the claim. Repeat this process as needed. Then, click (or tap) Add.

-
To attach an image from the document manager, click (or tap) Add From Document Manager. In the Add From Document Manager dialog box, select the checkboxes of the images that you want to attach, and select a classification/type for each selected image (if necessary, you can change the classification/type later by selecting a different option from the Classification/Type list on the Attachments tab). Click (or tap) Done.

-
To attach a perio exam, click (or tap) Add Perio Exam to view a menu that lists the dates of the patient's perio exams, and then click (or tap) the date of the perio exam that you want to attach.
-
To attach a narrative, click (or tap) Add Narrative to view a menu that lists the patient's clinical notes, and then click (or tap) the clinical note that you want to attach.
-
To remove attachments, select the All checkbox to select all the attachments, or select the checkboxes of the attachments that you want to remove. Click (or tap) Remove Selected. On the confirmation message that appears, click (or tap) OK.
Notes:
-
The Add Image button is available only if the payer is a supported carrier (a carrier that was added to your practice database from the list of supported carriers that Henry Schein maintains). The payer ID of an unsupported carrier is 06126.
-
The Add From Document Manager button is available only if the payer is a supported carrier (a carrier that was added to your practice database from the list of supported carriers that Henry Schein maintains). The payer ID of an unsupported carrier is 06126.
-
The Add Perio Exam button is available only if the patient has perio exams entered in his or her record and if the payer is a supported carrier (a carrier that was added to your practice database from the list of supported carriers that Henry Schein maintains). The payer ID of an unsupported carrier is 06126.
-
The Add Narrative button is available only if the patient has clinical notes entered in his or her record and if the payer is a supported carrier (a carrier that was added to your practice database from the list of supported carriers that Henry Schein maintains). The payer ID of an unsupported carrier is 06126.
-
You can attach images from a patient's document manager only if those images are .jpg/.jpeg files. You can attach only one perio exam to any given claim, but you can attach a perio exam to multiple claims. If you attach a clinical note as a narrative, Dentrix Ascend automatically converts it to a .jpg file.
-
You can have up to a total of 10 attachments per claim, but the total claim size (claim data and attached files) must be smaller than 15 MB.
-
-
Status/Notes
The Status/Notes tab displays the status of the claim, the created and sent (if applicable) dates of the claim, the original reference number, and status notes. Some notes are entered automatically, such as a status message with an attachment ID if the claim has attachments.

If an update for the status of the claim has not been received from the clearinghouse for at least two days, the Refresh Status button is available. To request an immediate update, click (or tap) the button. However, manually requesting an update should not be needed under normal circumstances. If the request results in a status change, the new status appears next to Status, and a note regarding the update appears in the Notes list. Also, the Refresh Status button becomes unavailable, but may become available again after two days without an update from the clearinghouse has elapsed.
Enter or change the Payer Claim Reference # provided by the payer (to replace or void the claim, the reference number is required). To resubmit the claim with the changes (replacing the original claim), click (or tap) Replace Claim. To void the claim (enter a zero payment), click (or tap) Void Claim. You can access a replaced or voided claim from the patient's Insurance Claims page.
To add a custom status update, click (or tap) Add Note, enter a message in the Note box, and then click (or tap) the Completed button
 .
.
-
-
Do one of the following:
-
To save the changes, click (or tap) Save. If you have made certain changes to the claim (added or removed procedures on the Procedures tab or made changes to the accident information on the Claim Info tab), and if the claim is already matched to an ERA, a confirmation message appears. To confirm that you want to save the changes and unmatch the claim, click (or tap) Proceed. Then, to close the claim dialog box, click (or tap) Cancel.
-
To save the changes and submit the claim, click (or tap) Submit.
-
To save the changes and resubmit the claim, click (or tap) Resubmit.If you have made certain changes to the claim (added or removed procedures on the Procedures tab or made changes to the accident information on the Claim Info tab), and if the claim is already matched to an ERA, a confirmation message appears. To confirm that you want to save the changes and unmatch the claim, click (or tap) Proceed.
-
If the claim does not have any electronic attachments, to create a .pdf file of the claim, which you can print, click (or tap) Print. A confirmation message appears. If you have made certain changes to the claim (added or removed procedures on the Procedures tab or made changes to the accident information on the Claim Info tab), and if the claim is already matched to an ERA, the claim will become unmatched if you print the claim. To proceed, click (or tap) Print.
Note: Printing a claim with a Queued status will stop the claim from being sent to the carrier.
-