Validating subscriber IDs
To help with insurance eligibility verification, when you are adding or editing a patient's insurance plan, you can have Dentrix Ascend attempt to validate the subscriber ID and let you know if the subscriber is eligible or not eligible or if there is some kind of error that needs to be addressed. This validation process is just a quick status check to give you advanced notice of a patient's status without having to schedule an appointment.
Notes:
-
Validating a subscriber ID requires the "Request Eligibility" security right.
-
This validation process is available only for primary plans.
-
This validation process is supported only if the payer supports standard data (Eligibility Essentials) requests. Even if the payer supports enhanced data (Eligibility Pro) requests, if it does not support standard data (Eligibility Essentials) requests, the validation will fail and display a "Payer ID Not Supported" error.
-
This validation process does not provide a breakdown of the patient's eligibility for coverage. A .pdf file with eligibility details is not saved to the patient's Document Manager, and an option to import insurance details is not available. Those eligibility details are available only for eligibility verifications that are performed for scheduled appointments (see the topics about verifying eligibility statuses and importing insurance information).
Refer to the following table for a comparison between validating subscriber IDs and verifying eligibility statuses.
Validating Subscriber ID
Verifying Eligibility Status
Purpose
Quick status check
Full eligibility verification
Usage
Adding an insurance plan to a patient's record
Viewing a patient's scheduled appointment
Plan Availability
Primary plan only
Primary plan only
PDF With Breakdown
No
Yes
Save to Document Manager
No
Yes
Import Insurance Information
No
Yes
To validate a subscriber ID
-
Do one of the following:
-
Click the Check Subscriber ID button
 next to the Subscriber ID # box.
next to the Subscriber ID # box.
During the check, a progress indicator appears below the Subscriber ID# box.

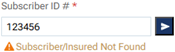
When the check is complete, one of the following occurs:
-
If there is a problem getting a response or determining eligibility (due to a timeout issue or another error), an orange triangle icon and a message with a description of the error (such as "Subscriber/Insured Not Found" or "Payer ID Not Supported") appear.
-
If the subscriber is not eligible, a red triangle icon and the message "Subscriber Not Eligible" appear.

-
If the subscriber is eligible, a green checkmark icon and the message "Subscriber Eligible" appear.

-
If the payer does not support electronic eligibility verification, a blue "I" icon and the message "Insurance Doesn’t Support Electronic Eligibility" appear.

-
-
Specify or change any other insurance information as needed.
-
If you are attaching insurance to the patient, or if you have changed any of the patient's insurance information, click (or tap) Save.