

The Ledger window provides a wealth of insurance information at a glance. For example, if a patient has insurance coverage, the Insurance menu is available. If the Insurance menu is unavailable, you have not assigned insurance to the patient in the Family File.
Note: If the Insurance menu is unavailable, but the selected patient has insurance, from the Ledger click View and clear All (with running balance).
From the Transaction Log, you can quickly determine the status of a procedure or claim. The Ins column indicates whether you have billed a procedure to insurance. If the column is empty, the listed procedure is attached to an insurance claim. If "No" appears in the Ins column, you have not created an insurance claim.
Once you create a dental insurance claim, the Outstanding Billed to Insurance, Expected from Dental Insurance, and Guarantor Portion of Total Balance amounts change to reflect the amount of the claimed procedures and the insurance coverage percentages.
Note: The insurance estimates in the Ledger and on Billing Statements only include procedures that you have billed to dental insurance. Dentrix allocates the entire procedure cost to the guarantor portion until you create a dental claim for the procedure.
You can create pre-treatment estimates from the Ledger’s Treatment Plan view. In addition to indicating whether a pre-treatment estimate has been created, the Ins column indicates the status of the estimate. "Acc" in the column means that the procedure has been pre-authorized. "Rej" indicates that the procedure has been rejected.
An insurance claim or a pre-treatment estimate has a status in the description of the transaction log. The following statuses are possible:
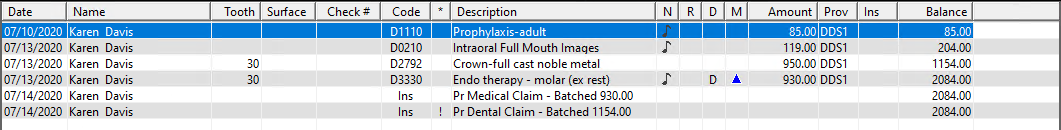
· Created - Identifies a claim that has been created but not yet processed.
· Batched - Identifies a claim that has been created and sent to the Batch Processor.
· Printed - Identifies a claim that has been created and printed from the Ledger.
· e Sent - Identifies a claim that has been submitted electronically to eClaims from the Ledger.