The Transaction Summary Report lists financial transactions (charges, payments, credit adjustments, charge adjustments, finance charges, and late charges) that have been posted to Ledger.
|
Why: |
To print a record of transactions each day, to review transactions for a date or date range, and to ensure transaction totals balance out over a variety of reports |
When: |
Daily |
To generate the report
In DXOne Reporting, select Analysis, and then double-click Transaction Summary Report.
The Transaction Summary Report dialog box appears.

Set up the following options:
Date Range - To filter the report by date, do one of the following:
To include transactions that have dates (based on the Date Type) within a range that you specify, select the Specific Range option. With this option selected, do one of the following:
Enter a date range (in a m/d/yyyy format) in the From and To boxes.
To select a date, do the following for From and To:
Click the corresponding calendar icon to view a month calendar.
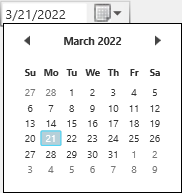
Navigate to the correct month using the left and right arrows.
Note: To quickly change the year and month, click the month-year at the top of the calendar, navigate to the correct year using the left and right arrows, and then click the correct month.
Click the correct day.
To include transactions that have dates (based on the Date Type) within a range that is relative to the report date, select the Relative Date Range option. With this option selected, select one of the following relative date ranges from the list:
Current Day Current MTD Current Fiscal YTD Current Calendar YTD |
Previous Day Previous Week Previous Month Previous 3 Months Previous 6 Months Previous Fiscal Year Previous Calendar Year |
Date Type - Select one of the following options:
Entry Date - To include a transaction based on the date that it was created (entered into the database).
Procedure Date - To include a transaction based on the date that was specified for it.
Notes:
Most of the time, a transaction will have the same entry and procedure date. They will differ only if you backdate the transaction.
Applied credits are included based on the allocate date instead of the entry or procedure date. So, credits that have been applied within the date range for the report will appear on the report even if the date of the credit is not within the date range for the report. For example, a payment dated 4/8/2022 can be partially applied on 4/9/2022. If the report is run for 4/9/2022, grouping by provider, the applied portion of the payment will appear (with the 4/8/2022 date). However, any suspended amount will not appear.
Clinic - To filter the report by the clinics that are associated with transactions (based on either the collecting or rendering clinic), do one of the following:
To include all clinics that you are allowed to generate the report for, select the All checkbox.
To include specific clinics, do the following:
Click the search button  .
.
The Select Clinics dialog box appears.

Note: Only the clinics that you are allowed to generate the report for are available.
If the list is long, to search for a clinic by ID and/or title, do the following:
Click Search.
The options for searching appear in the upper list.

Enter the first character or more of a clinic's ID and/or title in the ID and Practice Title boxes, respectively.
Click Show Results to view a list of matching clinics.
Note: To return to viewing the list of all the clinics, click Search, click Clear Search to clear the search criteria that you entered, and then click Show Results.
In the upper list, select one or more clinics.
Note: To select multiple clinics, click a clinic, and then, while pressing the Ctrl key, click the other desired clinics. To select a range of adjacent clinics, click the first clinic of the desired range of clinics, and then, while pressing the Shift key, click the last clinic of the desired range of clinics.
Click Add.
Repeat steps b-d as needed to add other clinics.
Note: To remove a clinic that you added, select that clinic in the lower list, and then click Remove.
Click OK.
Also, select one of the following options:
Collecting Clinic - To include transactions according to the following criteria:
A credit (applied or suspended) may appear on the report if its collecting clinic is one of the specified clinics for the report.
A charge may appear on the report if its rendering clinic is one of the specified clinics for the report.
Rendering Clinic - To include transactions according to the following criteria:
An applied credit may appear on the report if the rendering clinic of the charge that it's applied to is one of the specified clinics for the report.
A suspended credit may appear on the report if its collecting clinic is one of the specified clinics for the report.
A charge may appear on the report if its rendering clinic is one of the specified clinics for the report.
Provider/Staff - To filter the report by the providers that are associated with transactions, do one of the following:
To include all providers that you are allowed to generate the report for, select the All checkbox.
To include specific providers, do the following:
Click the search button  .
.
The Select Providers/Staff dialog box appears.

Note: Only the providers and staff that you are allowed to generate the report for are available.
If the list is long, to search for a provider by ID, first name, last name, and/or title, do the following:
Click Search.
The options for searching appear in the upper list.

Enter the first character or more of a provider's ID, first name, last name, and/or title in the ID, First Name, Last Name, and Title boxes, respectively.
Click Show Results to view a list of matching providers and staff members.
Note: To return to viewing the list of all the providers and staff members, click Search, click Clear Search to clear the search criteria that you entered, and then click Show Results.
In the upper list, select one or more providers.
Note: To select multiple providers, click a provider, and then, while pressing the Ctrl key, click the other desired providers. To select a range of adjacent providers, click the first provider of the desired range of providers, and then, while pressing the Shift key, click the last provider of the desired range of providers.
Click Add.
Repeat steps b-d as needed to add other providers.
Note: To remove a provider that you added, select that provider in the lower list, and then click Remove.
Click OK.
Notes:
An applied credit may appear on the report if the rendering provider of the charge that it's applied to is one of the specified providers for the report.
A charge may appear on the report if its rendering provider is one of the specified providers for the report.
If you run the report for all providers, a suspended credit may appear on the report. However, if you specify particular providers for the report instead of running it for all providers, suspended credits will not appear on the report regardless of the selected Group By option.
Billing Type - To filter the report by the billing types that are associated with patients who have transactions entered in their records, do one of the following:
To include all billing types, select the All checkbox.
To include specific billing types, do the following:
Click the search button  .
.
The Select Billing Type dialog box appears.

If the list is long, to search for a billing type by ID and/or description, do the following:
Click Search.
The options for searching appear in the upper list.

Enter the first character or more of a billing type's ID and/or description in the ID and Description boxes, respectively.
Click Show Results to view a list of matching billing types.
Note: To return to viewing the list of all the billing types, click Search, click Clear Search to clear the search criteria that you entered, and then click Show Results.
In the upper list, select one or more billing types.
Note: To select multiple billing types, click a billing type, and then, while pressing the Ctrl key, click the other desired billing types. To select a range of adjacent billing types, click the first billing type of the desired range of billing types, and then, while pressing the Shift key, click the last billing type of the desired range of billing types.
Click Add.
Repeat steps b-d as needed to add other billing types.
Note: To remove a billing type that you added, select that billing type in the lower list, and then click Remove.
Click OK.
Patient Age - To filter the report by patient ages, do one of the following:
To include patients of any age, select the All checkbox.
To include patients of specific ages, do the following:
Click the search button  .
.
The Select Ages dialog box appears.

Note: Ages 1 through 120 are available.
To search for an age by number or description, do the following:
Click Search.
The options for searching appear in the upper list.

Either enter a number in the ID box, or type Age followed by a space and then a number in the Age box.
Click Show Results to view a list of matching ages.
Note: To return to viewing the list of all the ages, click Search, click Clear Search to clear the search criteria that you entered, and then click Show Results.
In the upper list, select one or more ages.
Note: To select multiple ages, click an age, and then, while pressing the Ctrl key, click the other desired ages. To select a range of adjacent ages, click the first age of the desired range of ages, and then, while pressing the Shift key, click the last age of the desired range of ages.
Click Add.
Repeat steps b-d as needed to add other ages.
Note: To remove an age that you added, select that age in the lower list, and then click Remove.
Click OK.
ADA Code - To filter the report by the procedures that have been entered into patient records, do one of the following:
To include all procedure codes, select the All checkbox.
To include specific procedure codes, do the following:
Click the search button  .
.
The Select ADA Codes dialog box appears.

Do one of the following:
To get a list of all procedure codes, do not enter any search criteria.
To search for procedure codes by category, abbreviated description, ADA code, and/or description, enter the first character or more of a procedure code category, abbreviated description, ADA code, and/or ADA description in the Category, User Code, ADA Code, and/or Description boxes, respectively.

Click Show Results to view a list of matching procedure codes.

Note: To clear the search criteria that you entered so you can search again, click Search, and then click Clear Search. Then, repeat steps b-c.
In the upper list, select one or more procedure codes.
Note: To select multiple procedure codes, click a procedure code, and then, while pressing the Ctrl key, click the other desired procedure codes. To select a range of adjacent procedure codes, click the first procedure code of the desired range of procedure codes, and then, while pressing the Shift key, click the last procedure code of the desired range of procedure codes.
Click Add.
Repeat steps b-e as needed to add other procedure codes.
Note: To remove a procedure code that you added, select that procedure code in the lower list, and then click Remove.
Click OK.
Payment - To filter the report by payment type, do one of the following:
To include all payment types, select the All checkbox.
To include specific payment types, do the following:
Click the search button  .
.
The Select Payment Types dialog box appears.
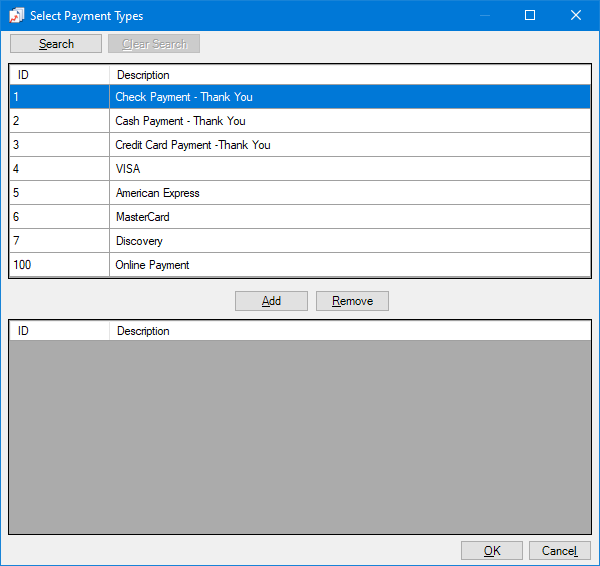
If the list is long, to search for a payment type by ID and/or description, do the following:
Click Search.
The options for searching appear in the upper list.
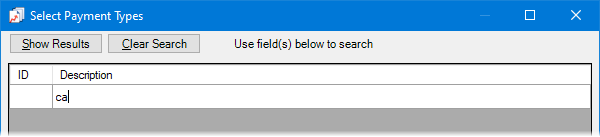
Enter the first character or more of a payment type's ID and/or description in the ID and Description boxes, respectively.
Click Show Results to view a list of matching payment types.
Note: To return to viewing the list of all the payment types, click Search, click Clear Search to clear the search criteria that you entered, and then click Show Results.
In the upper list, select one or more payment types.
Note: To select multiple payment types, click a payment type, and then, while pressing the Ctrl key, click the other desired payment types. To select a range of adjacent payment types, click the first payment type of the desired range of payment types, and then, while pressing the Shift key, click the last payment type of the desired range of payment types.
Click Add.
Repeat steps b-d as needed to add other payment types.
Note: To remove a payment type that you added, select that payment type in the lower list, and then click Remove.
Click OK.
Adjustment - To filter the report by adjustment type, do one of the following:
To include all adjustment types, select the All checkbox.
To include specific adjustment types, do the following:
Click the search button  .
.
The Select Adjustment Types dialog box appears.

If the list is long, to search for an adjustment type by ID and/or description, do the following:
Click Search.
The options for searching appear in the upper list.

Enter the first character or more of an adjustment type's ID and/or description in the ID and Description boxes, respectively.
Note: The first character of a description is either a plus sign (+) for a debit adjustment or a dash (-) for a credit adjustment.
Click Show Results to view a list of matching adjustment types.
Note: To return to viewing the list of all the adjustment types, click Search, click Clear Search to clear the search criteria that you entered, and then click Show Results.
In the upper list, select one or more adjustment types.
Note: To select multiple adjustment types, click an adjustment type, and then, while pressing the Ctrl key, click the other desired adjustment types. To select a range of adjacent adjustment types, click the first adjustment type of the desired range of adjustment types, and then, while pressing the Shift key, click the last adjustment type of the desired range of adjustment types.
Click Add.
Repeat steps b-d as needed to add other adjustment types.
Note: To remove an adjustment type that you added, select that adjustment type in the lower list, and then click Remove.
Click OK.
Insurance Carrier - To filter the report by patients' primary dental insurance carriers, do one of the following:
To include transactions for patients with any primary dental insurance carrier, select the All checkbox.
To include transactions for patients with specific primary dental insurance carriers, do the following:
Click the search button  .
.
The Select Insurance Carrier dialog box appears.

If the list is long, to search for insurance carriers by name, group plan name, group plan number, and/or local number, do the following:
Click Search.
The options for searching appear in the upper list.

Enter the first character or more of an insurance carrier name, group plan name, group plan number, and/or local number in the Carrier Name, Group Plan, Group#, and Local# boxes, respectively.
Click Show Results to view a list of matching insurance carriers.
Note: To return to viewing the list of all the insurance carriers, click Search, click Clear Search to clear the search criteria that you entered, and then click Show Results.
In the upper list, select one or more insurance carriers.
Note: To select multiple insurance carriers, click an insurance carrier, and then, while pressing the Ctrl key, click the other desired insurance carriers. To select a range of adjacent insurance carriers, click the first insurance carrier of the desired range of insurance carriers, and then, while pressing the Shift key, click the last insurance carrier of the desired range of insurance carriers.
Click Add.
Repeat steps b-d as needed to add other insurance carriers.
Note: To remove an insurance carrier that you added, select that insurance carrier in the lower list, and then click Remove.
Click OK.
Patient Tag - Do one of the following:
To not filter the report by a patient tag, clear the Run By Patient Tag checkbox.
To filter the report by the tags that are assigned to patients, select the Run By Patient Tag checkbox. With this checkbox selected, the options to filter the report by tag are available. Do one of the following:
To include transactions for patients with any patient tag, select the All checkbox.
To include transactions for patients with specific tags, do the following:
Click the search button ![]() .
.
The Patient Tag Selection dialog box appears.

If the list is long, to search for a patient tag, do the following:
Click Search.
The options for searching appear in the upper list.

Enter the first character or more of a patient tag name in the Tag Name box.
Click Show Results to view a list of matching patient tags.
Note: To return to viewing the list of all the patient tags, click Search, click Clear Search to clear the search criteria that you entered, and then click Show Results.
In the upper list, select one or more patient tags.
Note: To select multiple patient tags, click a patient tag, and then, while pressing the Ctrl key, click the other desired patient tags. To select a range of adjacent patient tags, click the first patient tag of the desired range of patient tags, and then, while pressing the Shift key, click the last patient tag of the desired range of patient tags.
Click Add.
Repeat steps b-d as needed to add other patient tags.
Note: To remove a patient tag that you added, select that patient tag in the lower list, and then click Remove.
Click OK.
Group By - Select one of the following options:
No Group By - For no grouping. Only the grand totals appear on the report. The totals are not broken down by clinic or provider.
Clinic - To group the report by clinic. The totals are broken down by clinic, and the report displays grand totals.
Do one of the following:
To not group the report by provider within each clinic grouping, clear the Provider checkbox. The report displays a charge with its associated rendering clinic. The report displays a suspended credit with its associated collecting clinic. The report displays an applied credit with either the rendering clinic of the charge that it's applied to or its collecting clinic.
To group the report by provider within each clinic grouping, select the Provider checkbox. For each provider, the report displays totals that are related to the outer clinic grouping. The report displays a charge with its associated rendering provider. The report displays a suspended credit under a "SUSPENDED CREDITS" grouping. The report displays an applied credit with the rendering provider of the charge that it's applied to.
Provider - To group the report by provider. Totals are broken down by provider, and the report displays grand totals.
Do one of the following:
To not group the report by clinic within each provider grouping, clear the Clinic checkbox. The report displays a charge with its associated rendering provider. The report displays an applied credit with the rendering provider of the charge that it's applied to. With this grouping option, the report does not display suspended credits because suspended credits are not associated with a provider.
To group the report by clinic within each provider grouping, select the Clinic checkbox. For each clinic, the report displays totals that are related to the outer provider grouping. The report displays a charge with its associated rendering clinic. The report displays an applied credit with either the rendering clinic of the charge that it's applied to or its collecting clinic. With this grouping option, the report does not display suspended credits because suspended credits are not associated with a provider.
Report Type - Select one of the following options:
Full Report - The report lists transactions, includes grand totals, and may include totals by clinic or provider (depending on the selected Group By option).
Summary Report - The report includes grand totals and may include totals by clinic or provider (depending on the selected Group By option).
Click Save as Default to save the current settings for the next time you run the report.
Click Clear Defaults to revert the dialog box options to the original defaults.
Click Schedule to schedule a report job.
Click OK to preview the report.

Important information this report provides
The report can be grouped and subtotaled by provider with a breakdown by clinic. Or, the report can be grouped and subtotaled by clinic with a breakdown by provider. The following information can be used to monitor production for each provider and/or clinic.
Transactions - The transactions posted to Ledger.
Transaction Details - Each transaction provides the following information:
Entry Date or Procedure Date - According to the selected Date Type for the report, the date that a transaction was created, or the specified service date of a procedure.
Patient Name - The patient’s name.
Patient Age - The patient's age.
Insurance - The patient's primary dental insurance carrier.
Description - The ADA code and description, or transaction description.
Charges or Credits - Any charges or credits.
BT - Billing type.
Provider - The ID of the provider who is associated with the transaction.
Clinic - The clinic where the transaction was posted.
Grand Totals - The following information appears in the Grand Totals section:
Charges and Adjustments - The total amounts billed to insurance, charged to patients, and adjusted on an account.
Balances - The balance prior to the date of the day sheet, the balance for the date of the day sheet, and the net change between the two balances.
Payments - The total amounts of payments received from insurance and patients or adjusted on an account.
Average Prod Per Patient - The average value of procedures per patient (the total charged for procedures divided by the total number of patients seen).
Average Chg Per Procedure - The average charge per procedure (the total charged for procedures divided by the total number of procedures performed).
Provider Totals - The transactions are shown for the provider with a breakdown of the procedures for each clinic the provider works in. Each clinic’s transactions for that provider are subtotaled. The transaction totals for the provider appear below the clinic subtotals.
Clinic Totals - The transactions are shown for the clinic with a breakdown of the procedures performed by each provider at that clinic. Each provider’s transactions and suspended credits for that clinic are subtotaled. The transaction totals for the clinic appear below the provider subtotals.