Indemnity: Participating dental plans
Charging office full fee and posting an adjustment at time of insurance payment
This is a dental insurance plan that the office DOES participate with, BUT the office wants to charge the fees from the default fee schedule and post an adjustment for the difference between the office fee and the allowable amount when the insurance payment is posted. Use the same settings as with "Indemnity: Non-participating Dental Plans":
General
Carrier – Enter the insurance company's name.
Employer – Enter the employer or group plan name.
Note: If the plan is an individual plan, enter "Individual" here.
Group – Enter the group number if applicable.
Plan – Select Indemnity.
Benefits and Limits:
Benefits – Select a benefit renewal option.
Maximum – Enter the maximum benefit.
Renew on – Enter the renewal date.
Estimates - Percents:
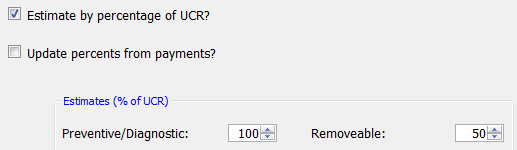
Estimate by percentage of UCR? – Select this check box.
Update percents from payments? – Clear this check box.
Estimates (% of UCR) – Enter the percentages by category.
Note: You can enter 0% to not estimate insurance portions or 100% to assign all of an amount to insurance.
Estimates - Estimator:
Use estimate in estimator – Select this option to enter code by code the amount that is expected from insurance or, if Update Estimator from payments? is selected, to use the amount that the program has learned.
Estimator – Click this button to enter codes for which you know the exact amount that the insurance will reimburse or to enter code-specific requirements, such as an X-ray being required when submitting a claim.
Note: You can add codes into the estimator only AFTER the insurance profile has been saved.
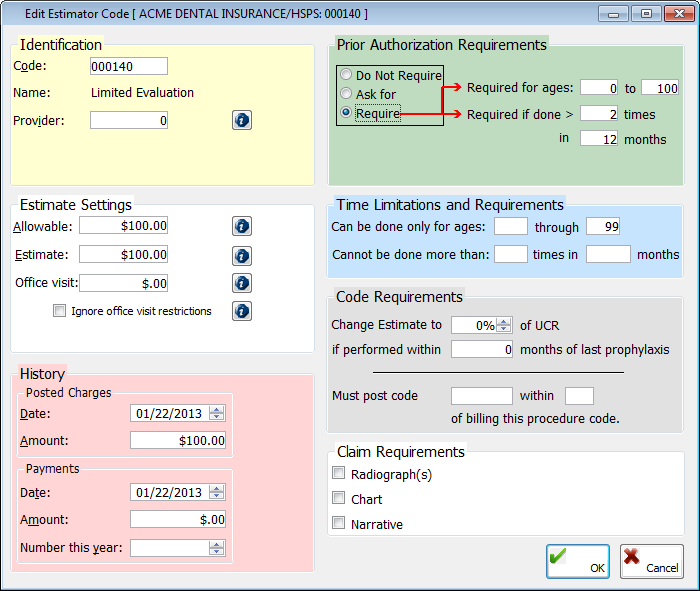
To add a code to the estimator table, do the following:
Click Add.
Type internal Code, or double-click to select one from the fee schedule.
Select a Provider to limit which doctor this estimate applies to.
Enter the Estimate amount. This is the amount that you expect the insurance carrier to pay for this procedure.
Enter any code-specific settings for the plan, such as claim requirements.
Claims (basic)
Claims (advanced)
Put which amount on claim – Select Amount Billed.