Estimator code settings
Set up the following options for an estimator code:
Identification:
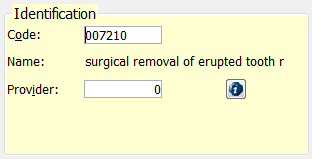
Code – Type the internal code from the fee schedule, or double-click to select the code.
Name – This is the name of the procedure code as it appears in the fee schedule. If the name DOES NOT appear after you enter the code, that code is not recognized, and you must re-enter the code.
Provider – Type the provider number of the provider for whom these estimator settings apply. Type zero (0) if there is only one doctor in the practice, or if these settings apply to ALL doctors in the practice.
Note: You can enter the same code multiple times if there are different allowables or settings per provider.
Estimate Settings:
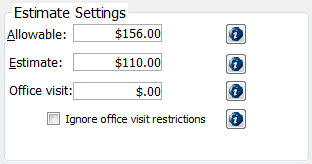
Allowable – Type the maximum amount that the insurance company allows for this procedure. This amount is VERY important for PPO, DMO, and Managed Care plans as this is the amount that will be charged to the patient when you are posting charges or treatment planning (as long as this fee is equal to or less than the office's fee). This amount defaults to the office's fee, and for Indemnity plans, you can leave the office fee entered or replace it with the insurance allowable if known.
Estimate – Type the amount that the insurance company will reimburse the office for this procedure. The charged amount minus this estimate will be the patient's estimated portion.
Office Visit – Type the office visit fee, or co-pay. This not the patient portion of the billed procedures but an additional charge (which will appear in the Ledger as a separate line item). Typically, with managed care plans, there is no direct patient portion per procedure, so the patient must pay a co-pay.
Note: The system can charge the highest, lowest, or all co-pays associated with the codes being posted. This can be set up in the insurance profile on the Estimates-Estimator tab.
Ignore office visit restrictions – To override whether the highest or lowest co-pay for this procedure should be charged, select this check box.
History:
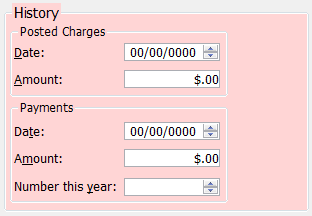
Posted Charges – This displays the last date and amount this code was posted to any patient.
Payments – This displays the last date and payment amount received from this plan for this procedure. It also displays the total number of payments received from this plan for this code.
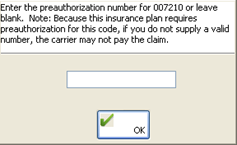
Prior Authorization Requirements:
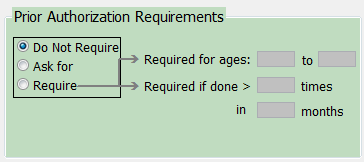
Do not require – Select this check box if prior authorization is not recommended or required for this procedure.
Ask for – Select this check box if prior authorization is recommended but not required for this procedure. When you post this procedure, a dialog box will appear and ask you for the prior authorization number.

Require – Select this check box if prior authorization is required for this procedure.
Required for ages # to # – Enter the age range within which prior authorization is required. Enter 0 to 100 for all ages.
Required if done in ># times in # mos – Enter a frequency limit where prior authorization is required. (for example, if this code is performed more than 2 times in 60 months).
When you post this procedure, a dialog box will appear and ask you for the prior authorization number.
Time Limitations & Requirements:
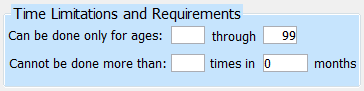
Can only be done for ages # through # – Enter the age range within which this procedure will be covered (for example, fluoride for ages 0 tthrough 12).
Cannot be done more than # times in # months – Enter a frequency limitation in which the procedures will be covered (for example, an adult prophy cannot be done more than 2 times in 12 months).
Code Requirements:
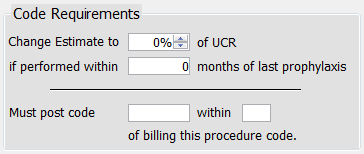
Change estimate to % of UCR if performed within # months of last prophylaxis – Enter the percentage at which this procedure will be covered if performed within the specified number of days since the patient's last prophy.
Must post code X within # of billing this procedure code – Enter the procedure code that must be posted within a set number of days after this procedure in order for it to be covered.
Claim Requirements:
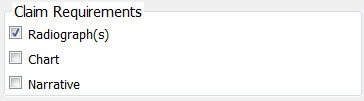
Radiograph(s) – Select this check box if X-rays are required when sending a claim with this procedure code.
Chart – Select this check box if periodontal charting is required when sending a claim with this procedure code.
Narrative – Select this check box if a narrative is required when sending a claim with this procedure code.
Note: These will appear on a claim requirements report, which can be run by opening the Report menu, pointing to Daily, and then clicking Claim Requirements.
Need more help?
You can visit our website or contact OMSVision Customer Support.
