DMO: Participating dental plans
Flat fee schedule plans
This is a dental insurance plan that the office DOES participate with. The contracted rate (insurance allowable) will be charged to a patient, and the different employer or group plans pay based on a flat fee. Any procedure code that has not been entered into the estimator table will be charged at the full office rate, and the estimated patient portion will be the full amount.
Step 1 - Create DMO plan profile
In the Insurance Profiles window, click Add.
Set up the following options:
General:
Carrier – Enter the insurance company's name (for example, Aetna).
Employer – Enter plan name (for example, Plan L).
Plan – Select DMO.
Benefits and Limits:
Default Fee Schedule – Select "<Use Default>."
Estimates - Percents:
Estimate by percentage of UCR? – Select this check box.
Update percents from payments? – Clear this check box.
Estimates (% of UCR) – Enter zero percent for ALL categories.
Note: Any procedure code NOT in the estimator will NOT have an estimated insurance portion, and the patient will be responsible for the amount in full.
Estimates - Estimator:
Use estimate in Estimator – Select this check box.
Update Estimator from payments? – Clear this check box.
Claims (basic)
Claims (advanced):
Put which amount on claim – Select Fee in Fee Schedule (UCR).
Click OK to save profile
Step 2 - Enter insurance contracted rates (allowables) and fee schedule
Note: For any procedure NOT in the estimator table, the patient will be charges the office's UCR fee, and the estimated patient portion will be the full amount.
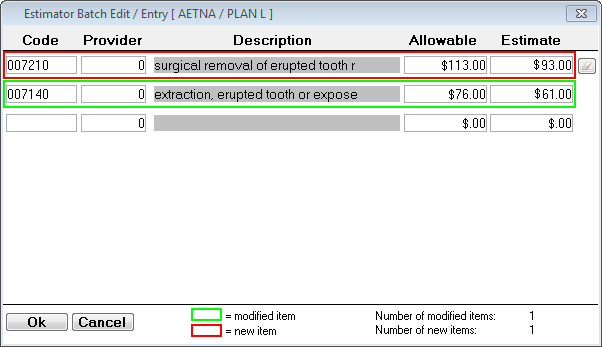
In the Insurance Profiles window, select the plan profile (for example, Aetna Plan L), and then click Estimator.
Click Batch Edit.
Note: You can also use the Add and Import options.
Type a Code. This is the internal, 6-character code from the master fee schedule.
Note: Codes in red boxes are new codes that will be added to the estimator. Codes in green boxes already exist in the estimator but will be updated.
Type a Provider number. Use zero if the allowable applies to ALL providers.
Note: You can set up billing groups to enter allowables based on a grouping of providers such as by specialty. If you use billing groups, do NOT use the Batch Edit method as it does not allow you to attach a billing group to each procedure.
Type the Allowable amount.
For the Estimate, type the amount that the insurance company will pay the office.
Note: The difference between the Allowable and the Estimate amounts is the patient portion.
Repeat steps A–F for all codes.
Click OK.