When you enter an insurance payment for a primary dental insurance claim, if the patient has additional coverage, Dentrix Enterprise prompts you to create a secondary dental insurance claim. However, if you chose to not create a secondary dental insurance claim after posting the primary dental insurance payment, or if you attached a secondary dental insurance plan to the patient's record or updated that plan after creating the primary dental insurance claim, you can manually create a secondary dental insurance claim. Likewise, you can create a tertiary dental insurance claim after posting a secondary dental insurance payment, and you can create a quaternary dental insurance claim after posting a tertiary dental insurance payment.
Additionally, for a secondary dental insurance claim, you must enter the details from the Claim Adjustment Segment (CAS)/Coordination of Benefits (COB) of the primary dental insurance claim. If the secondary claim has been created automatically, or if you manually create the secondary claim, you must edit it to provide these details to prevent the claim from being rejected.
Note:
Viewing insurance claims requires the "Insurance Claims, Open" security right. Creating insurance claims requires the "Insurance Claims, Create New" security right.
Editing subscriber information (to update Dentrix Enterprise to use new secondary dental insurance plan information) requires the "Insurance Claims, Edit" security right.
To create and edit a secondary dental insurance claim
Open the Primary Dental Insurance Claim window if it is not already open.

If you attached a secondary dental insurance plan to the patient's record or updated that plan after creating the primary dental insurance claim, you must update Dentrix Enterprise to use the new secondary dental insurance plan information to create a secondary dental insurance claim. Do the following:
Double-click the Subscriber Information block.
If applicable, do one of the following:
If the Password - Insurance Claims, Edit dialog box appears, user verification has been assigned to the "Insurance Claims, Edit" task. Do one of the following:
If your user account has been granted the "Insurance Claims, Edit" security right, enter your credentials in the User ID and Password boxes, and then click OK.
If your user account has not been granted the "Insurance Claims, Edit" security right, have a user with permission temporarily override this restriction so you can edit subscriber information this one time. The overriding user enters his or her credentials in the User ID and Password boxes and then clicks OK.

If a message appears, informing you that you do not have rights to this operation, your user account has not been granted the "Insurance Claims, Edit" security right. To have a user with permission temporarily override this restriction so you can edit subscriber information this one time, do the following:
On the message, click Yes.

In the Password - Insurance Claims, Edit dialog box, the overriding user enters his or her credentials in the User ID and Password boxes and then clicks OK.

The Patient/Insurance Information dialog box appears.

Select the Update Secondary Insurance checkbox.
Click OK.
You are returned to the Primary Dental Insurance Claim window.
To create the secondary dental insurance claim, on the Claim menu, click Create Secondary Dental.
If applicable, do one of the following:
If the Password - Insurance Claims, Create New dialog box appears, user verification has been assigned to the "Insurance Claims, Create New" task. Do one of the following:
If your user account has been granted the "Insurance Claims, Create New" security right, enter your credentials in the User ID and Password boxes, and then click OK.
If your user account has not been granted the "Insurance Claims, Create New" security right, have a user with permission temporarily override this restriction so you can create a claim this one time. The overriding user enters his or her credentials in the User ID and Password boxes and then clicks OK.

If a message appears, informing you that you do not have rights to this operation, your user account has not been granted the "Insurance Claims, Create New" security right. To have a user with permission temporarily override this restriction so you can create a claim this one time, do the following:
On the message, click Yes.

In the Password - Insurance Claims, Create New dialog box, the overriding user enters his or her credentials in the User ID and Password boxes and then clicks OK.

Dentrix Enterprise creates the secondary dental insurance claim, and the Secondary Dental Insurance Claim window opens.

Note: After creating the secondary dental insurance claim, you can easily switch back and forth between the primary and secondary dental insurance claims by clicking View Primary Dental or View Secondary Dental on the Claim menu.
Double-click the Claim Information block.
Note: The Claim Information block displays "Standard" until the information has been changed; in which case, it will display "Non-Standard."
If applicable, do one of the following:
If the Password - Insurance Claims, Edit dialog box appears, user verification has been assigned to the "Insurance Claims, Edit" task. Do one of the following:
If your user account has been granted the "Insurance Claims, Edit" security right, enter your credentials in the User ID and Password boxes, and then click OK.
If your user account has not been granted the "Insurance Claims, Edit" security right, have a user with permission temporarily override this restriction so you can change standard claim information this one time. The overriding user enters his or her credentials in the User ID and Password boxes and then clicks OK.

If a message appears, informing you that you do not have rights to this operation, your user account has not been granted the "Insurance Claims, Edit" security right. To have a user with permission temporarily override this restriction so you can change standard claim information this one time, do the following:
On the message, click Yes.

In the Password - Insurance Claims, Edit dialog box, the overriding user enters his or her credentials in the User ID and Password boxes and then clicks OK.

The Insurance Claim Information dialog box appears.
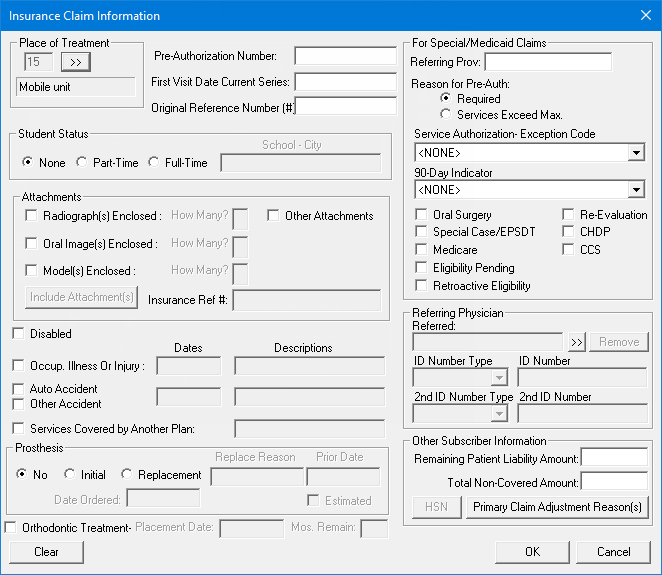
For the secondary claim, you must enter the details from the Claim Adjustment Segment (CAS)/Coordination of Benefits (COB) of the primary claim. You must use the CAS segment to report the primary carrier's claim level adjustments that cause the amount paid to differ from the amount originally charged.
Note: If you do not add primary claim adjustment reasons, the secondary claim will likely be rejected with an error message such as "COB claim balancing failed total charge amount," "Claim amount does not equal sum of paid amount and all adjustment amounts," or "Other Carrier Claim Out of Balance." This rejection message is due to the absence of, or invalid information in, the CAS segment, which is used to represent primary claim adjustments. Adjustment information is intended to help the secondary payor balance the remittance information. Adjustment amounts should fully explain the difference between the submitted charges and the amount paid by the primary insurance carrier.
To add a primary claim adjustment reason to the secondary claim, do the following:
Under Other Subscriber Information, click Primary Claim Adjustment Reason(s).
Click the button.
The Primary Claim Adjustment Reason(s) dialog box appears.

Note: All of the information that the codes represent should be reflected on the ERA/EOB from the primary insurance payor. However, the codes themselves might not appear on a paper remittance. (Refer to the X12 standards website for more information on the possible codes.)
From the Group Code list, select one of the following options:
CO: Contractual Obligations - The amount of the adjustment is not the patient's responsibility under any circumstances due to either a contractual obligation between the payor and provider or a regulatory requirement.
CR: Correction and Reversals, - The claim is the reversal of a previously reported claim or claim payment.
OA: Other adjustments - If no other category is applicable for the adjustment.
PI: Payor Initiated Reductions - In the payor's opinion, the amount of the adjustment is not the patient's responsibility without a supporting contract between the payor and provider.
PR: Patient Responsibility - The amount of the adjustment is the patient's responsibility.
In the Reason Code box, enter a code (two to five characters in length).
Notes:
If you use a code from 1-9, make sure that you include a leading zero when you enter the code (01-09).
Use the following guidelines for specifying a reason code:
01, 02, or 03 - Use only with PR (Patient Responsibility).
18 - Use only with OA (Other Adjustment) except where state workers' compensation requires CO (Contractual Obligations).
23 - Use only with OA (Other Adjustment).
45 - Use only with PR (Patient Responsibility) or CO (Contractual Obligations) depending upon liability.
85 - Use only with PR (Patient Responsibility).
133 - Use only with OA (Other Adjustment).
136 - Use only with OA (Other Adjustment).
201 - Use only with PR (Patient Responsibility).
209 - Use only with OA (Other Adjustment).
229 - Use only with PR (Patient Responsibility).
238 - Use only with PR (Patient Responsibility).
249 - Use only with CO (Contractual Obligations).
255 - Use only with OA (Other Adjustment).
257 - Use only with OA (Other Adjustment).
P3 - Use only with PR (Patient Responsibility).
P11 - Use only with OA (Other Adjustment).
P16 - Use only with CO (Contractual Obligations) or OA (Other Adjustment).
W5 - Use only with CO (Contractual Obligations) or OA (Other Adjustment).
In the Amount box, enter the amount of the adjustment (negative or positive, from -99,999,999.99 to 99,999,999.99) that was made to the primary claim.
Click Add.
Click Close.
Under Other Subscriber Information, in the Remaining Patient Liability Amount box, enter the patient portion from the ERA/EOB from the primary insurance payor. This amount should be total amount billed on the primary claim minus the sum of the primary claim payment and adjustments (from the CAS segment).
Note: The remaining patient liability must equal the amount being billed to the secondary payor. In other words, if you subtract the primary claim payment, the primary claim adjustments (from the CAS segment), and the remaining patient liability amount from the total amount billed on the primary claim, the balance must be zero (0). For example:
Total billed to primary = $100
Primary claim payment = -$70
Primary claim adjustments = -$10
Remaining patient liability = -$20
Balance = $0
Change other standard claim information for the secondary dental insurance claim as needed.
Click OK.
Additionally, edit the secondary dental insurance claim as needed.