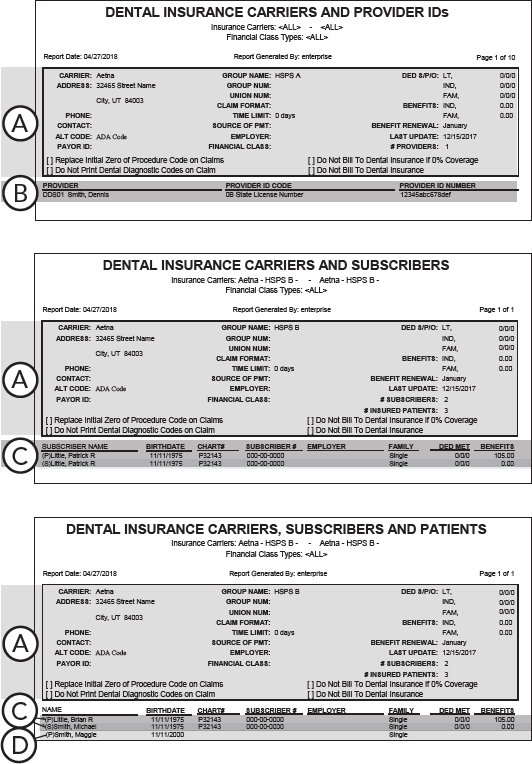
The Insurance Carrier List displays a list of the dental/medical insurance carriers entered in Dentrix Enterprise. Depending on how you run the report, the subscribers and patients, or providers that are associated with each carrier can also appear on this report.
|
Why: |
To ensure insurance carriers are properly set up in Dentrix Enterprise |
When: |
After Dentrix Enterprise setup, and as needed |
To generate the report
In DXOne Reporting, select Reference, and then double-click Insurance Carrier List.
The Insurance Carrier List dialog box appears.

Note: You cannot filter the report by clinic, so the Clinic options are not available.
Set up the following options:
Insurance Carrier - To filter the report by insurance carrier, do one of the following:
To include all insurance carriers, select the All checkbox for both From and To.
To include a specific range of insurance carriers, select the starting insurance carrier (alphabetically by name) of the range for From and the ending insurance carrier of the range for To.
To include a specific insurance carrier, select the same insurance carrier for both From and To.
To include an open-ended range of insurance carriers, select an insurance carrier for either From or To, and then select the All check box for the other option.
To select a specific insurance carrier for From or To, do the following:
Click the corresponding search button
 .
.
The Select Insurance Carriers dialog box appears.

Do one of the following:
To get a list of all insurance carriers, do not enter any search criteria.
To search for insurance carriers by name, group plan name, group plan number, local number, payor ID, and/or address, enter the first character or more of an insurance carrier name, group plan name, group plan number, local number, payor ID, and/or address in the Carrier Name, Group Plan, Group#, Local#, Payor ID, and Address boxes, respectively.

Note: To clear any text that you have entered, click Clear Search.
Click Show Results to view a list of insurance carriers.

Note: To clear the list so you can search again, click Search.
In the list, select an insurance carrier.
Click OK.
Financial Class Options - Select one of the following options:
Display Plans with no Financial Class type assigned - To display insurance carriers whose plans do not have financial classes assigned to them.
Selected Financial Class Types - To display insurance carriers whose plans have specific financial classes assigned to them.
If the Selected Financial Class Types option is selected, to filter the report by the class types that are assigned to plans that are provided by insurance carriers, do one of the following:
To include all class types, select the All checkbox.
Note: This checkbox is available only if the Selected Financial Class Types option is selected.
To include specific class types, do the following:
Click
the search button ![]() .
.
Note: This button is available only if the Selected Financial Class Types option is selected.
The Select Financial Class dialog box appears.

If the list is long, to search for a class type by ID and/or description, do the following:
Click Search.
The options for searching appear in the upper list.

Enter the first character or more of a class type's ID and/or description in the ID and Description boxes, respectively.
Click Show Results to view a list of matching class types.
Note: To return to viewing the list of all the class types, click Search, click Clear Search to clear the search criteria that you entered, and then click Show Results.
In the upper list, select one or more class types.
Note: To select multiple class types, click a class type, and then, while pressing the Ctrl key, click the other desired class types. To select a range of adjacent class types, click the first class type of the desired range of class types, and then, while pressing the Shift key, click the last class type of the desired range of class types.
Click Add.
Repeat steps b-d as needed to add other class types.
Note: To not include a class type that you added, select that class type in the lower list, and then click Remove.
Click OK.
Insurance Type - To filter the report by the type of insurance that carriers provide, select one of the following options:
Dental - To include insurance carriers that are associated with dental insurance plans.
Medical - To include insurance carriers that are associated with medical insurance plans.
Report Options - Select one of the following options:
Standard List - To generate the list of insurance carriers.
With this option selected, you can include additional details on the report. Optionally, select one of the following checkboxes:
Include Subscribers - To list the subscribers of plans that are provided by insurance carriers on the report.
Include All Patients - To list the subscribers and patients who are covered under plans that are provided by insurance carriers on the report.
Include Provider IDs - To list the providers with IDs that have been set up for plans that are provided by insurance carriers on the report.
Note: To not include additional details, make sure a checkbox is not selected.
Mailing Labels - To generate mailing labels for the insurance carriers.
Label Type - If the Mailing Labels option is selected under Report Options, select the option that corresponds to the type of label sheets that you use: Avery 5351 (3x11) or Avery 5160 (3x10).
Note: These options are available only if the Mailing Labels option is selected.
Click Save as Default to save the current settings for the next time you run the report.
Click Clear Defaults to revert the dialog box options to the original defaults.
Click Schedule to schedule a report job.
Click OK to preview the report.
Important information this report provides
The report includes insurance carrier details. When setting up options to run the report, you can choose to also include subscribers, subscribers and patients, or providers on the report.
Insurance Carrier Details:
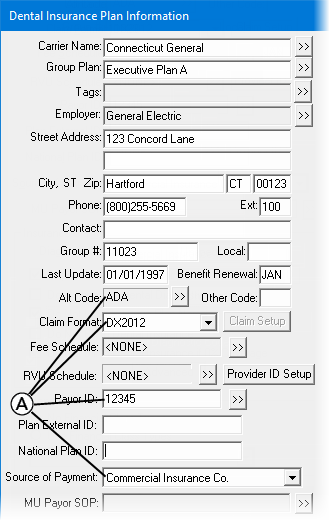
The following information is found in the Dental Insurance Plan Information or Medical Insurance Plan Information dialog box:
Claim Format - The claim form that is used to send printed claims.
Alt Code - Indicates whether ADA or alternate procedure codes are used when claims are sent to an insurance carrier (dental only).
Payor ID - A unique number that is used to identify an insurance carrier for claims that are submitted electronically. Payor IDs are updated regularly by the eServices clearinghouse.
Source of Payment - The category that is used to identify payments that are received from the insurance carrier.
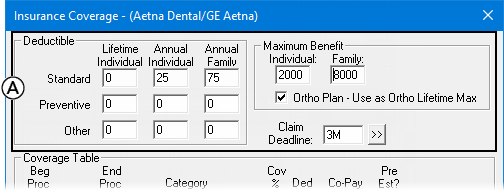
The following information is found in the Insurance Coverage dialog box (dental only):
Claim Deadline - The number of days/weeks/months/years in which a claim must be submitted to the insurance carrier.
Ded S/P/O:
LT - The lifetime deductible of a policy (if any).
Ind - The annual deductible for an individual.
Fam - The annual deductible for a family.
Benefits:
Ind - Yearly benefits for individuals.
Fam - Yearly benefits for families.
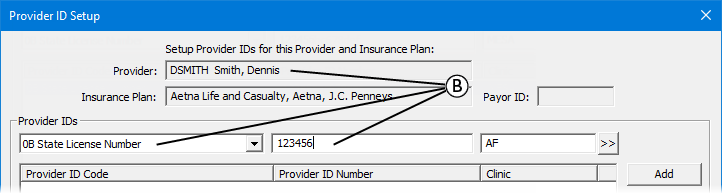
Provider Details - The name, ID code, and ID number for each provider with an identification code that has been entered for a plan provided by an insurance carrier. This information is found in the Provider ID Setup dialog box.
Subscriber Details - The name, birth date, chart number, subscriber number, employer, and family status of each subscriber. The report also includes the portion of the subscriber’s deductible that has currently been met and the total benefits that have been used year-to-date.
Notes:
"(P)" indicates a primary subscriber. "(S)" indicates a secondary subscriber.
If the report includes subscribers and patients, subscribers are denoted with an asterisk (*).
Patient Details - The name, birth date, chart number, employer, and family status for each patient associated with the insurance carrier. The report also includes the portion of the patient’s deductible that has currently been met and the total benefits that have been used year-to-date.
Notes:
"(P)" indicates a primary subscriber. "(S)" indicates a secondary subscriber.
If the report includes subscribers and patients, subscribers are denoted with an asterisk (*).