Most insurance companies provide the patient with a schedule of benefits, which declares the maximum annual benefits for the individual and entire family. The schedule of benefits also states the deductible amounts, plan maximums, and the percentage of the usual and customary fee that the insurance company will pay. You can add this information to an insurance plan as a coverage table. You can also specify the deadline for submitting any claim and select the applicable method to calculate insurance co-payments. A coverage table helps you create treatment plan estimates that accurately reflect the benefits that an insurance carrier will pay.
Notes:
You can also edit dental coverage information in Family File.
Changing an insurance plan's coverage affects all subscribers and patients who are covered under the plan.
Changing coverage information requires the "Insurance Coverage, Modify" security right.
To change the coverage table for a dental insurance plan
In the Insurance Maintenance dialog box, leave the Dental tab selected.
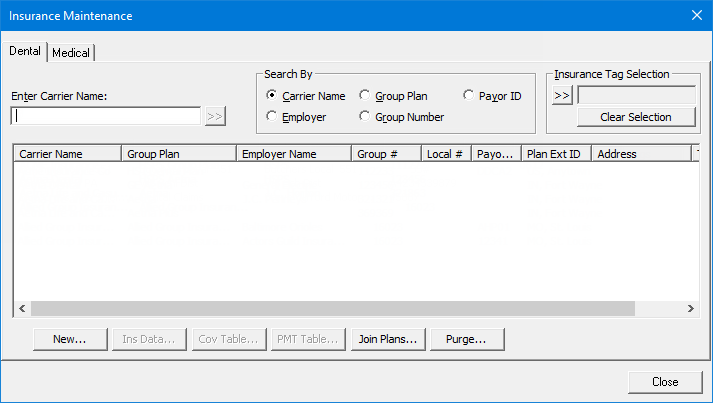
To search for an insurance plan, do the following:
To search for plans that have particular insurance tags, do the following:
Under Insurance
Tag Selection, click the search button ![]() .
.
The Insurance Tag Selection dialog box appears.
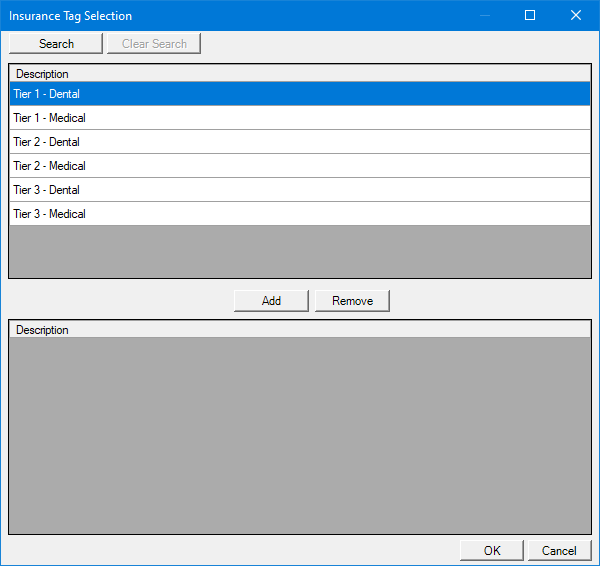
Note: If the upper list is long, to filter it by name, click Search, enter all or the first part of a tag name, and then click Show Results to view the matches.
In the upper list, select the desired tags.
Note: To select multiple tags, click a tag, and then, while pressing the Ctrl key, click the other desired tags. To select a range of adjacent tags, click the first tag of the desired range of tags, and then, while pressing the Shift key, click the last tag of the desired range of tags.
Click Add.
The selected tags now appear in the lower list.
Note: To remove a tag from the lower list, select it, and then click Remove.
Click OK.
Note: To clear all the selected insurance tags at one time, click Clear Selection.
Under Search By, select one of the following options:
Carrier Name - To search by carrier name.
Employer - To search by employer name.
Note: This option is available only if an employer has already been assigned to the current patient.
Group Plan - To search by group plan name.
Group Number - To search by group plan number.
In the Enter Carrier Name, Enter Employer Name, Enter Group Plan Name, or Enter Group Number box (the name varies according to the selected Search By option), enter all or part of a carrier name, employer name, group plan name, or group plan number, respectively.
Click
the search button ![]() .
.
Any matching insurance plans appear in the list.
Select an insurance plan.
Click Cov Table.
The Insurance Coverage dialog box appears. The carrier and group plan name appear on the title bar for your reference.
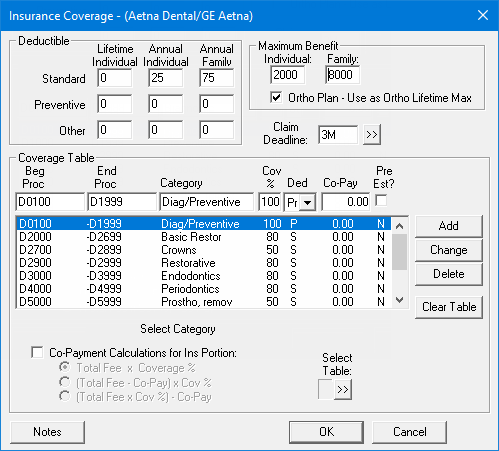
Set up the following options as needed:
Deductible - Each range of procedure codes in your coverage table can be associated with a deductible type. The following types of deductibles are available:
Standard (S) - Use for most insurance plans.
Preventive (P) - Use if an insurance plan's coverage has a separate deductible for preventive/diagnostic procedures.
Other (O) - Use if an insurance plan's coverage has a separate deductible for specific procedures other than preventive/diagnostic.
For each type of deductible, you can specify the following amounts:
Lifetime Individual - Use for an insurance plan that requires subscribers to pay one deductible for an individual, insured person for the life of the subscriber's policy.
Annual Individual - Use for an insurance plan that requires each patient to pay a deductible amount each benefit year.
Annual Family - Use for an insurance plan that has a maximum deductible amount for an entire family each benefit year. The sum of the Annual Individual deductible amounts (if applicable) for all the insured people on the subscriber's policy may not exceed the Annual Family deductible.
Note: When Dentrix Enterprise calculates the patient's portion of charges, the applicable deductible amounts, if any, are factored into the Est. Patient Portion in Ledger.
Maximum Benefit:
Individual - The maximum amount that the insurance carrier will pay for an individual, insured person annually.
Family - The maximum amount that the insurance carrier will pay for all the insured people on the subscriber's policy annually.
Ortho Plan - Use as Ortho Lifetime Max - The maximum lifetime benefits for an orthodontic plan. With this check box selected, the maximum benefits for the Individual and Family are the maximum amounts that the insurance carrier will pay for the life of the subscriber's policy.
Claim Deadline - The length of time that is allowed by the insurance carrier for you to submit a pre-treatment estimate or claim before it expires and will not be accepted. Do one of the following:
In the box, type the number 1, 2, 3, 4, 5, or 6 and then the letter D (for day), W (for week), M (for month), or Y (for year). For example, type 1M for one month.
To select a length of time, do the following:
Click the search button ![]() .
.
The Deadline dialog box appears.

On the left, select one of the following options: 1, 2, 3, 4, 5, or 6.
On the right, select one of the following options: Day, Week, Month, or Year.
Click OK.
Coverage Table - A coverage table allows you to group several procedures into ranges and assign the percentage the insurance will pay. Dentrix Enterprise provides five standard coverage tables that you can modify in Office Manager to fit your specific insurance plan needs. When you assign a new insurance plan to a subscriber, Dentrix Enterprise automatically assigns the first standard coverage table to the plan. If you do not have or know the insurance company's schedule of benefits, as you make insurance payments and estimates in Ledger, Dentrix Enterprise will provide you the option to automatically update a payment table for the insurance plan, storing what the insurance company actually pays for a procedure. Insurance estimate calculations will reflect the payment table amounts whenever possible, making your estimates very accurate.
You can use one of the standard coverage tables as is or create a custom coverage table (for this plan only) based on one of the standard coverage tables. Do any of the following as needed:
To select a different coverage table, do the following:
Click the Select
Table search button ![]() .
.
The Select Coverage Table dialog box appears.
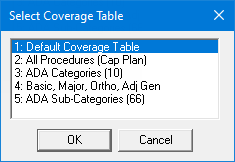
Select the coverage table that is most like the coverage table that is needed for configuring this insurance plan's coverage.
Click OK to copy the selected coverage table to this plan, overwriting the plan's original coverage table. You can modify the coverage as needed.
Note: If you need to modify the plan's coverage table, keep the following in mind:
You must use ADA Procedure Codes.
You may not overlap the beginning and ending procedure codes in any given range.
A procedure code can pertain to only one range.
To delete a procedure code range from the coverage table, do the following:
Select a procedure code range.
Click Delete.
To change a procedure code range of the coverage table:
Select a procedure code range.
Change any of the following options for the selected range:
Beg Proc - The beginning procedure code in the range.
End Proc - The ending procedure code in the range. If you are assigning only one procedure to a range, enter that procedure code in the Beg Proc box, and leave the End Proc box blank. The box will automatically be filled in with the beginning procedure code.
Category - A name to represent the range of procedure codes, such as an ADA Procedure Code Category name.
Cov % - The percentage the insurance carrier will pay for any of the procedures in the range.
Ded - The deductible type for the range of procedure codes.
Co-Pay - For a capitation plan, the patient's co-pay amount. If the plan is not a capitation plan, enter 0.00 in the box.
Pre Est? - Whether a pre-treatment authorization is required or not. If the insurance company requires you to submit a pre-treatment estimate for a procedure in the range, select this checkbox; otherwise, clear the checkbox.
Note: As you modify the plan's coverage table, keep the following in mind:
You must use ADA Procedure Codes.
You may not overlap the beginning and ending procedure codes in any given range.
A procedure code can pertain to only one range.
Click Change.
To add a procedure code range to the coverage table:
Select a procedure code range.
Change any of the following options for the selected range:
Beg Proc - The beginning procedure code in the range.
End Proc - The ending procedure code in the range. If you are assigning only one procedure to a range, enter that procedure code in the Beg Proc box, and leave the End Proc box blank. The box will automatically be filled in with the beginning procedure code.
Category - A name to represent the range of procedure codes, such as an ADA Procedure Code Category name.
Cov % - The percentage the insurance carrier will pay for any of the procedures in the range.
Ded - The deductible type for the range of procedure codes.
Co-Pay - For a capitation plan, the patient's co-pay amount. If the plan is not a capitation plan, enter 0.00 in the box.
Pre Est? - Whether a pre-treatment authorization is required or not. If the insurance company requires you to submit a pre-treatment estimate for a procedure in the range, select this checkbox; otherwise, clear the checkbox.
Note: As you modify the plan's coverage table, keep the following in mind:
You must use ADA Procedure Codes.
You may not overlap the beginning and ending procedure codes in any given range.
A procedure code can pertain to only one range.
Click Add.
Co-Payment Calculations for Ins Portion - If the plan requires that specific co-pay amounts be paid by the patient for each procedure, select this checkbox; otherwise, clear this check box.
Important: Select the Co-Payment Calculation for Ins Portion checkbox only if the plan that you are setting up is a capitation type plan with specific co-payment amounts for each procedure.
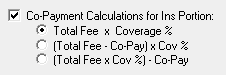
With this checkbox selected, select one of the following options to specify which method will be used to calculate the amount that the insurance company will pay:
Total Fee x Coverage %.
(Total Fee - Co-Pay) x Cov %.
(Total Fee x Cov%) - Co-Pay.
Notes - Notes regarding the insurance plan. For example, you can record special requirements that the insurance plan might impose.
Note: Insurance plan notes are available in any patient record that has this insurance plan attached to it. Also, insurance plan notes will appear in an insurance claim window but not on the corresponding claim. So, you can update the notes from a coverage table or a claim window as needed from any patient records with the same insurance plan.
To enter or change the insurance plan notes, do the following:
Click Notes.
The Insurance Plan Note dialog box appears.
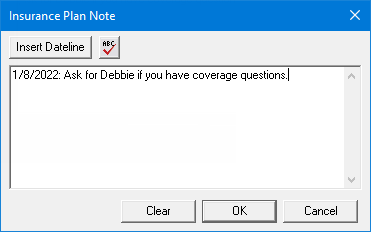
In the box, enter, delete, or change the text.
Notes:
To add a date stamp to the note where the text cursor is currently positioned in the box, click Insert Dateline.
To insert a blank line or start a new line in the box, while pressing Ctrl, press Enter.
To
check the spelling of the note text, click the Check
Spelling button, click the Check
Spelling button ![]() (this button is available only
if a certain preference
setting is enabled).
(this button is available only
if a certain preference
setting is enabled).
Click OK.
Click OK.
If applicable, do one of the following:
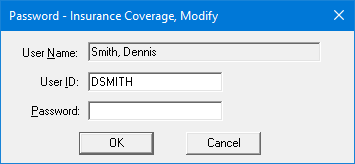
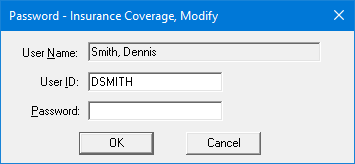
If the Password - Insurance Coverage, Modify dialog box appears, user verification has been assigned to the "Insurance Coverage, Modify" task. Do one of the following:
If your user account has been granted the "Insurance Coverage, Modify" security right, enter your credentials in the User ID and Password boxes, and then click OK.
If your user account has not been granted the "Insurance Coverage, Modify" security right, have a user with permission temporarily override this restriction so you can save the coverage information this one time. The overriding user enters his or her credentials in the User ID and Password boxes and then clicks OK.
If a message appears, informing you that you do not have rights to this operation, your user account has not been granted the "Insurance Coverage, Modify" security right. To have a user with permission temporarily override this restriction so you can save the coverage information this one time, do the following:
On the message, click Yes.
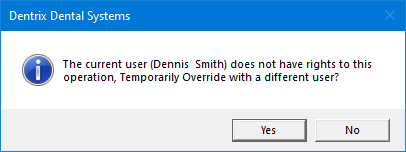
In the Password - Insurance Coverage, Modify dialog box, the overriding user enters his or her credentials in the User ID and Password boxes and then clicks OK.
A message appears, reminding you of the following: any changes will affect all subscribers and patients who are covered under this plan, and changes to the plan will affect any existing payment plan charges.
Click OK.