Clinical Quality Measures (CQMs) help providers assess treatment, processes, experience, and outcomes of patient care to help identify areas for quality improvement, identify differences in care/outcomes, and improve care coordination between providers.
For Dentrix Enterprise customers who are enrolled in the CQM solution, CQM data is copied from your Dentrix Enterprise database and stored on a CQM server at Henry Schein One. Using a a third-party web-based reporting tool called CQMsolution, you can run reports for the following six CQM measures:
68 Documentation of Current Medications in the Medical Record
74 Primary Caries Prevention Intervention as Offered by Primary Care Providers, Including Dentists
75 Children Who Have Dental Decay or Cavities
138 Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention
156 Use of High-risk Medications in the Elderly
165 Controlling High Blood Pressure
To enroll, contact Dentrix Enterprise Sales at 1-800-459-8067, option 1; for assistance with CQMsolution, contact Dentrix Enterprise Customer Support at 1-800-459-8067, option 2.
The Clinical Quality Measures List displays each Meaningful Use measure, the corresponding results (the population, the denominator and numerator used for calculating the actual percentage for a result, exclusions, and exceptions), and the details of the requirement for that measure.
|
Why: |
To view the calculated results of Meaningful Use clinical measures |
When: |
As needed |
Note: Accessing CQMsolution requires the "Clinical Quality Measures, Open" security right.
To open CQMsolution
In Office Manager, on the Analysis menu, point to Meaningful Use, and then click Clinical Quality Measures.
If applicable, do one of the following:
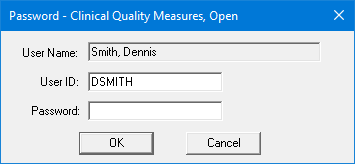
If the Password - Clinical Quality Measures, Open dialog box appears, user verification has been assigned to the "Clinical Quality Measures, Open" task. Do one of the following:
If your user account has been granted the "Clinical Quality Measures, Open" security right, enter your credentials in the User ID and Password boxes, and then click OK.
If your user account has not been granted the "Clinical Quality Measures, Open" security right, have a user with permission temporarily override this restriction so you can access CQMsolution this one time. The overriding user enters his or her credentials in the User ID and Password boxes and then clicks OK.
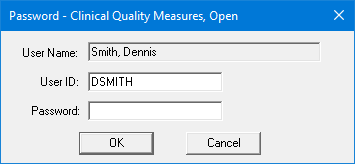
If a message appears, informing you that you do not have rights to this operation, your user account has not been granted the "Clinical Quality Measures, Open" security right. To have a user with permission temporarily override this restriction so you can access CQMsolution this one time, do the following:
On the message, click Yes.
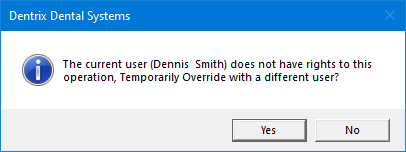
In the Password - Clinical Quality Measures, Open dialog box, the overriding user enters his or her credentials in the User ID and Password boxes and then clicks OK.
Before providers and staff can use CQMsolution, they will need to have their own user accounts set up.
To set up CQMsolution user accounts
After opening CQMsolution, on the Administration menu, click Users.
Click Add User.
The Add A New User page appears.
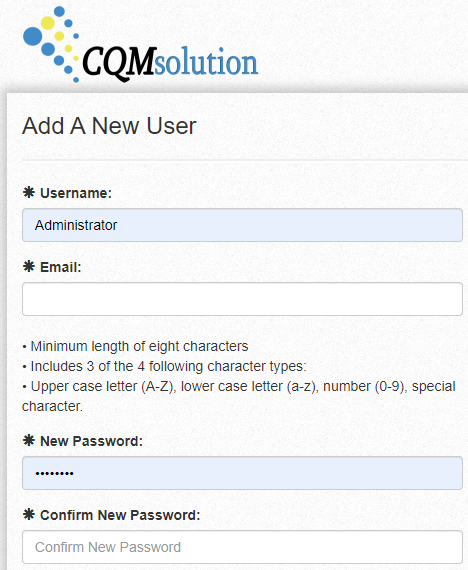
For the Username, enter the provider/staff ID that was used in the ID box for this provider/staff in Dentrix Enterprise. These IDs must match or the user will not be able to open CQMsolution from Dentrix Enterprise.
Fill in the other required information (marked with an asterisk) for the user, and then click Save.
To create and view a report
After opening CQMsolution, click Create Report.
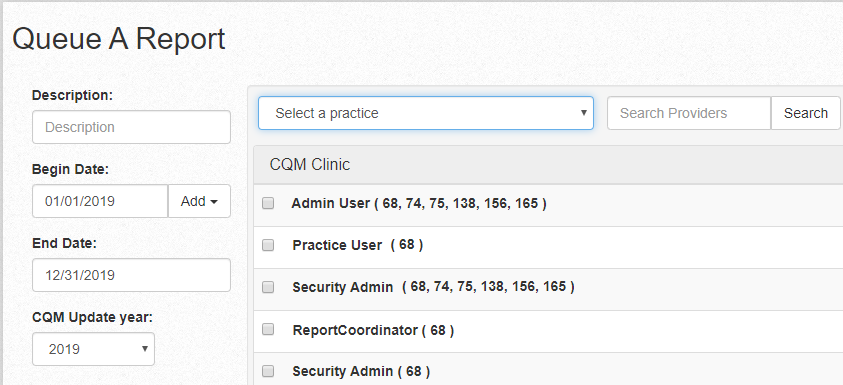
Enter a Description for the report.
If you have more than one practice, select a practice to use for this report.
Select a CQM report that includes the measures you want in your report.
Click Queue Report.
Your report appears at the top of the Queued Reports list.
To see the report results, click View Results.
The CQM report results include all the measures that were defined for the report.
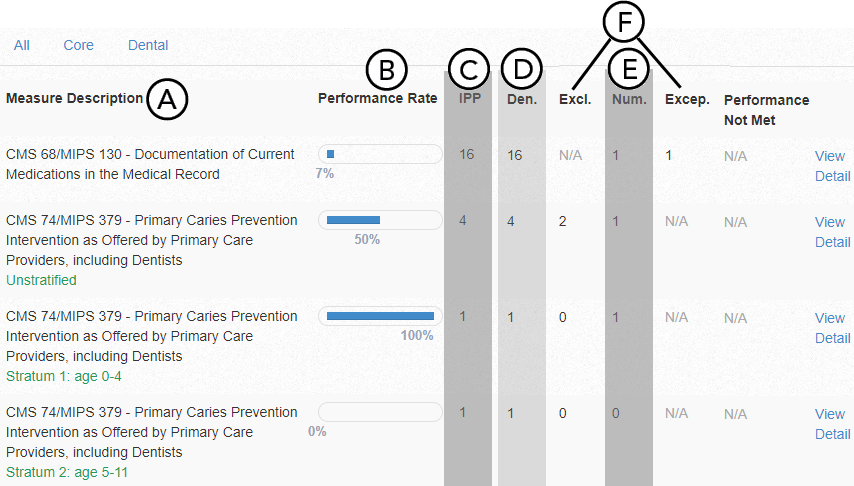
To view details of any of the measures in the report, click the corresponding View Detail link.
Important information this report provides
The CQM report results include all the measures that were defined for the report.
Measures - The list of measures.
Results - The calculated results.
Population - The patients.
Denominator - The denominator used in the calculation.
Numerator - The numerator used in the calculation.
Exclusions and Exceptions - Exclusions and exceptions that were not taken into account during the calculation.
The following tables explain the calculations and requirements for each measure.
68 Documentation of Current Medications in the Medical Record |
|
Requirement: Percentage of patient visits for patients aged 18 years and older for which the eligible professional (EP) attests to documenting a list of current medications using all immediate resources available on the date of the encounter. This list must include all known prescriptions, over-the-counter drugs, herbal supplements/medicines, and vitamin/mineral/dietary (nutritional) supplements and must contain the medications’ name, dosage, frequency, and route of administration. Exception: Patient is in an urgent or emergent medical situation where time is of the essence and to delay treatment would jeopardize the patient’s health status. |
|
Initial Patient Population |
The number of patients 18 years old or older before the start of the specified Measurement Period who have visits occurring during the 12-month reporting period. |
Denominator |
The number of patients in the Initial Patient Population. |
Numerator |
The number of patients (from the Denominator) for whom the EP attests to documenting a list of current medications for those patients. |
74 Primary Caries Prevention Intervention as Offered by Primary Care Providers, Including Dentists |
|
Requirement: Percentage of children who are less than 20 years of age and who received a fluoride varnish application during the specified Measurement Period. |
|
Initial Patient Population |
The number of children who are less than 20 years old with a visit during the specified Measurement Period. Stratum 1 - Patients 0 to 5 years old. Stratum 2 - Patients 6 to 12 years old. Stratum 3 - Patients 13 to 19 years old. |
Denominator |
The number of patients in the Initial Patient Population. |
Numerator |
The number of patients (from the Denominator) who receive a "Fluoride Varnish" (a procedure posted from the Chart with the appropriate CDT code). |
75 Children Who Have Dental Decay or Cavities |
|
Requirement: Percentage of children who are less than 20 years old who have tooth decay or cavities during the specified Measurement Period. |
|
Initial Patient Population |
The number of children who are less than 20 years old with a visit during the specified Measurement Period. |
Denominator |
The number of patients in the Initial Patient Population. |
Numerator |
The number of patients (from the Denominator) who have "Tooth Decay" or "Cavities" (a condition/diagnosis with the appropriate ICD-9-CM code). |
138 Preventive Care and Screening: Tobacco Use: Screening and Cessation Intervention |
|
Requirement: Percentage of patients aged 18 years or older who were screened for tobacco use one or more times within 24 months and who received cessation counseling intervention if identified as a tobacco user. Exception: Documentation of medical reason(s) for not screening for tobacco use (for example, limited life expectancy or other medical reason). |
|
Initial Patient Population |
All patients aged 18 years old or older. |
Denominator |
The number of patients in the Initial Patient Population. |
Numerator |
The number of patients (from the Denominator) who have been identified as a "Tobacco User" (a patient with the appropriate SNOMED-CT code) or "Non-Tobacco User" (a patient with the appropriate SNOMED-CT code) within 24 months of a patient’s health assessment or medical encounter being entered within the specified Measurement Period. |
156 Use of High-risk Medications in the Elderly |
|
Requirement: Percentage of patients 66 years of age or older who were ordered high-risk medications. |
|
Initial Patient Population |
Patients 66 years old or older who had a visit during the specified Measurement Period. |
Denominator |
The number of patients in the Initial Patient Population. |
Numerator 1 |
Patients with an order for at least one "High-risk Medication" (a prescription with the appropriate RxNorm code) during the specified Measurement Period. |
Numerator 2 |
Patients with an order for at least two different "High-risk Medications" (prescriptions with the appropriate RxNorm codes) during the specified Measurement Period. |
165 Controlling High Blood Pressure |
|
Requirement: The percentage of patients 18-85 years of age who had a diagnosis of hypertension and whose BP was adequately controlled during the measurement year. |
|
Initial Patient Population |
The number of patients who were 18 years old or older and less than or equal to 85 years old before the beginning of the specified Measurement Period. |
Denominator |
The number of patients in the Initial Patient Population who were diagnosed with "Hypertension" (a medical alert with the appropriate ICD-9-CM or SNOMED-CT code) up to 6 months after the specified Measurement Period and who have an "Encounter Outpatient" (a patient health assessment or medical encounter with the appropriate AMA-CPT code) with one of the selected Providers within the specified Measurement Period and who do not have one of the following: Evidence of end stage renal disease (ESRD) (an "active" medical alert with the appropriate ICD-9-CM or SNOMED-CT code). One or more procedures, such as dialysis or a renal transplant, that were performed for ESRD (a procedure posted from the Chart with the appropriate AMA-CPT code). Active diagnosis of "Pregnancy" (an "active" medical alert with the appropriate ICD-9-CM or SNOMED-CT code). "Encounter Pregnancy" (a medical encounter with the appropriate ICD-9-CM code). |
Numerator |
The number of patients (from the Denominator) who have had a diastolic blood pressure reading less than 90 mmHg and a systolic blood pressure reading greater than 140 mmHg during the most recent patient health assessment with one of the selected Providers within the specified Measurement Period. |