

The Claim Information block displays information that is specific to a patient and an insurance claim. The standard information prints on the claim unless you have edited it.
Note: By default, “Standard” appears in the Claim Information block. If you have changed the standard information, "Non-Standard” appears.
To change claim information
1. From the Ledger transaction log, double-click an insurance claim or payment or a preauthorization estimate.
The Insurance Claim or Preauthorization Estimate window appears.
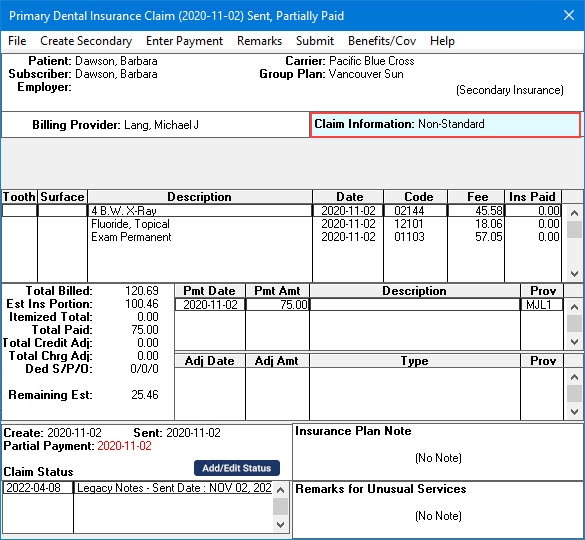
2. Double-click the Claim Information block.
The Insurance Claim Information dialog box appears.
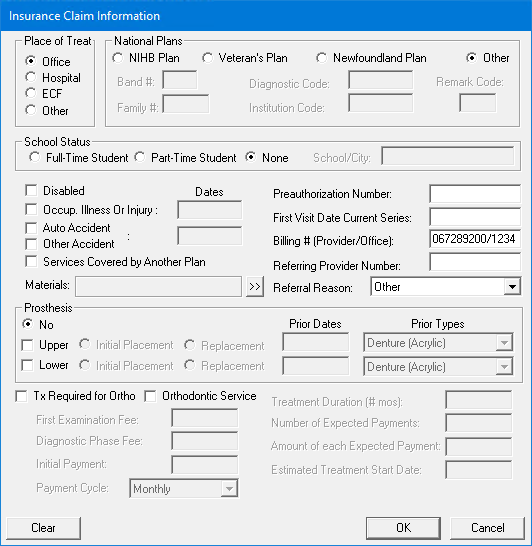
3. Make changes to any of the information displayed in the Insurance Claim Information dialog box:
Place of Treat - Select the location where treatment was performed.
National Plans - Select the appropriate national plan, and type the accompanying information for that plan.
School Status - Select the appropriate status for the patient. If the patient is a part- or full-time student, enter the name of the school and the city where it is located in the text box.
Disabled - Select if the patient is disabled.
Occupational Illness or Injury - Select if treatment was necessary due to an on-the-job illness or injury. Type the relevant date and description.
Accident Information - Select Auto Accident or Other Accident if treatment was necessary as result of an accident. Type the relevant date and description.
Services Covered by Another Plan - Select if needed and type a relevant description.
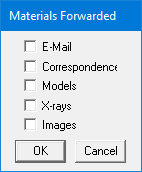
Materials - Click the search button (double chevron), and in the Materials Forwarded dialog box, select the supporting material that you will forward with the claim.
Pre-Authorization Number - If required, type the preauthorization number provided by the patient’s insurance carrier.
Note: If you received a preauthorization and entered it in Dentrix, the preauthorization number automatically prints on the insurance claim. If there is more than one number for the procedures on the claim, you must create a claim for each set of procedures with a different preauthorization number.
First Visit Date Current Series - Type the appropriate date.
Billing # (Provider/Office) - Type the billing number of the provider or office.
Referral - If treatment is being referred out, type a Referring Provider Number, and select a Referral Reason.
Prosthesis - If the claim involves a prosthesis, select the appropriate option and specify the necessary information.
Orthodontic Service - If the claim is for orthodontic service, specify the necessary information.
Note: To reset the Insurance Information options to the defaults, click Clear.
4. To save your changes and return to the Primary Dental Insurance Claim window, click OK.
Note: When you enter or clear claim information in a Claim window, the changes only apply to the currently displayed claim and the associated primary or secondary claim. When you create a new claim, the claim information uses the defaults for the current patient. You can change the defaults for the patient through the Appointment Book. For more information, click Scheduling appointments.