Wrap Around Claims Report
The Wrap Around Claims Report provides the necessary information for a Federally Qualified Health Center (FQHC) facility to petition Medicaid for supplemental payments. The report includes the number of encounters, rate, total amount billed, total receipts, and amount to be funded.
To generate the report
-
On the Home menu, under Reports, click (or tap) Power Reporting.
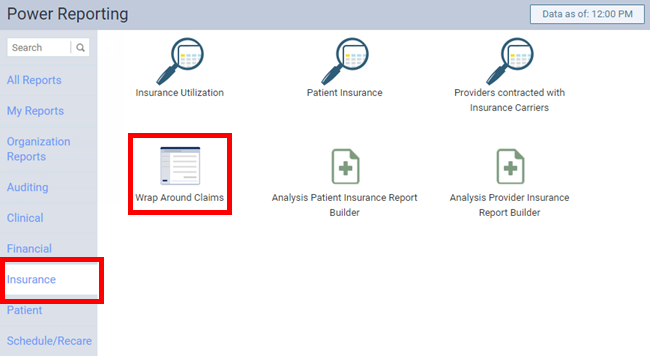
The Power Reporting page opens.
-
In the Insurance category, click (or tap) Wrap Around Claims.
The Wrap Around Claims page opens.
-
On the Wrap Around Claims page, set up the following options:
-
PPS Rate - The fixed amount of reimbursement through the Prospective Payment System (PPS) to report on.
-
Locations - The encounters in the selected locations. Do any of the following:
-
Select the All checkbox to include encounters in all locations in the organization. Or, clear the checkbox to not include encounters in any location in the organization.
-
Select or clear the checkbox next to the current location name to include or to not include the encounters in that location.
-
Click Select Locations to select or deselect locations.
-
-
Transaction Date Range - The date or date range of encounters to include on the report. Leave the previous quarter selected, or select the desired date (today or a specific date) or date range (previous week, previous month, previous six months, previous calendar year, or a custom range).
-
Provider - The provider of encounters to include on the report. Select whether you want the report to display encounters for all providers or a specific provider. Locations and business entities that have been set up as billing providers are also available for selection.
-
Claim Source of Payment - The source of payment assigned to insurance plans with claims for encounters to include on the report. Select whether you want the report to display encounters for any source of payment or a specific source of payment.
-
Claim Insurance Carrier - The insurance carrier of plans with claims for encounters to include on the report. Select whether you want the report to display encounters for any carrier or a specific carrier.
-
Claim Insurance Plan - The insurance plan with claims for encounters to include on the report. Select whether you want the report to display encounters for any plan or a specific plan.
-
-
Click (or tap) Search.
The report appears according to the specified rate and filters.

-
To print the report, click (or tap) Print.