Welcome to the quick start guide for Dentrix Eligibility Pro.
Dentrix Eligibility Pro simplifies the process of requesting insurance eligibility information with an integrated and automated workflow—all within Dentrix. You'll receive reliable, timely responses from top insurance payers, in a standardized form that's automatically saved to the Dentrix Document Center.
To get started, watch this video to become familiar with your new eligibility workflow (Duration 2:59).
Note: In this video, you'll see and hear references to Eligibility Essentials. Don't let that distract you. The routine daily workflow for Eligibility Essentials and Pro is much the same, though Eligibility Pro automatically searches payer portals and returns more information.
|
Have you recently purchased an Eligibility Pro subscription? Join our webinar and learn more about Eligibility Essentials and Eligibility Pro. Our onboarding team will assist you in getting started setting up your Payer Connection Portal to maximize the Pro features so you can begin receiving current, reliable and detailed eligibility data. |
|---|
To learn how to use Dentrix Eligibility Pro, click the topics below.
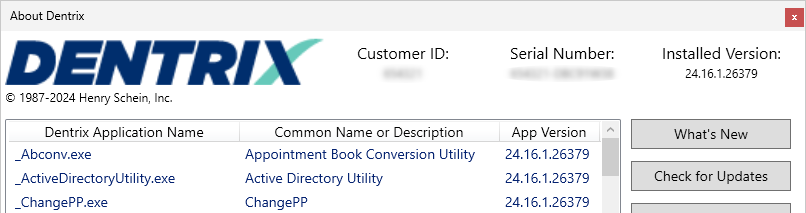
Make sure you're running Dentrix 24.16 or higher.
To check your Dentrix version, from the Help menu in any Dentrix module, click About Dentrix. You can see your version number in the upper-right corner of the About Dentrix window.
Verify that your eTrans account is active and properly configured. There are two ways that you can do this:
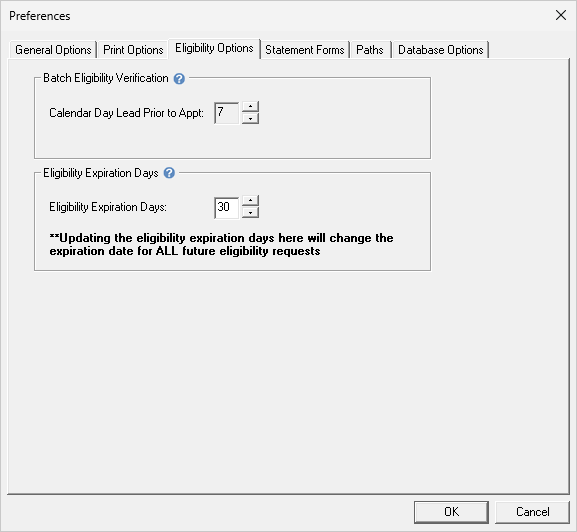
Setup your offices preferences for lead time and expiration of eligibility checks.
In Office Manager > Maintenance > Practice Setup > Preferences, and select the Eligibility Options tab. From the options presented, choose the following:
Eligibility Essentials submits the patient's information using the industry standard electronic data Interchange (EDI). No special credentials are necessary to make these requests.
With these requests, many carriers will send additional information with this check. Some carriers are generous with the information shared over an EDI request, but many are not. The amount and timeliness of the information can vary greatly from payer to payer.
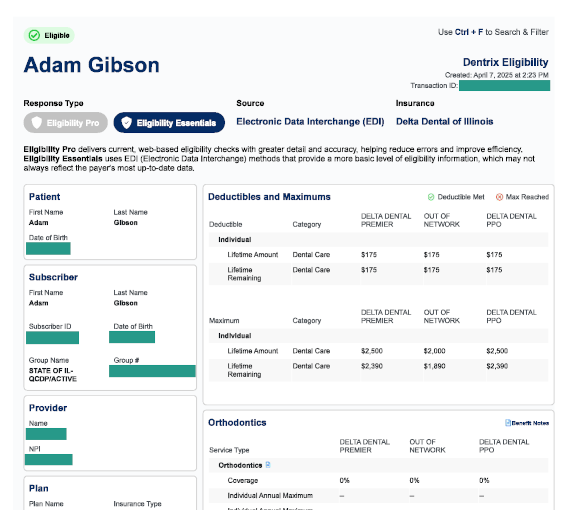
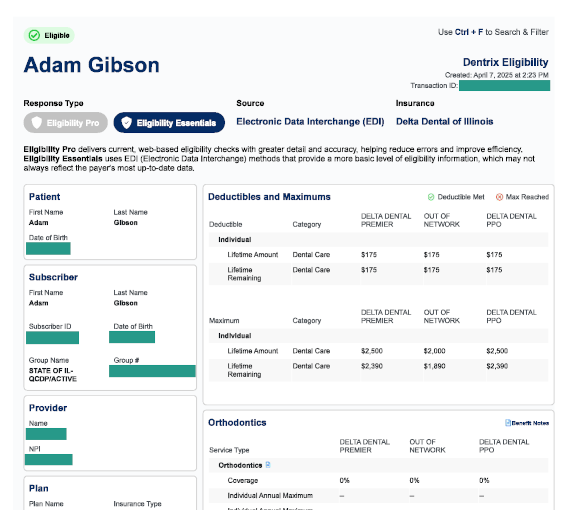
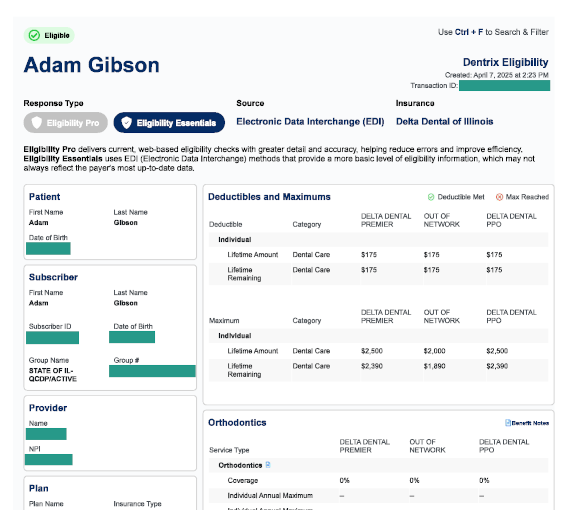
In this example response, the "Eligibility Essentials" bubble is darkened.
Because you're an Eligibility Pro customer, Dentrix will also check the insurance payer's web portal to get details that are only available there, such as patient history, frequency limitations, and procedure-level coverage percentages.
You'll need to set up your payer connections before you request an Eligibility Pro response for the first time. It's a simple process that gives Dentrix access to pull eligibility data from payer portals on your behalf.
Watch this short video to learn how to use the Payer Connection Portal (Duration 2:28).
For the latest update on how to establish a multi-factor authentication connection with the insurance carriers listed below, click the carrier name to open the configuration course in a new tab.
| Cigna | Delta Dental | Denti-Cal |
Registration for the listed carriers is not necessary. Enrollment will occur automatically when you send your first Eligibility Pro request for the carrier.
| Prinicpal | United Healthcare |
Eligibility requests occur automatically for appointments scheduled within the current month according to the amount of lead time you setup in Eligibility Options.
When you add an appointment within the lead-time window, Dentrix will check the patient's eligibility immediately.
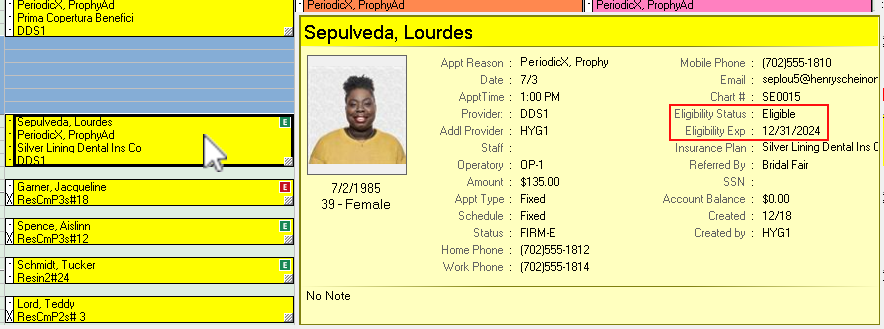
You can view a patient's eligibility status in the Appointment Book. The color of the letter "E" on each appointment means the following:
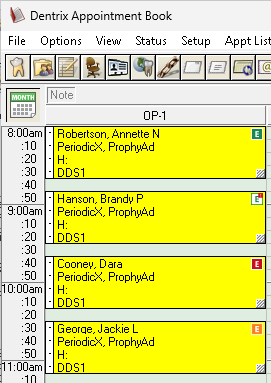
You also can view a patient's eligibility status in the Hover Window.
The color coded "E" can also be seen in the Family File.
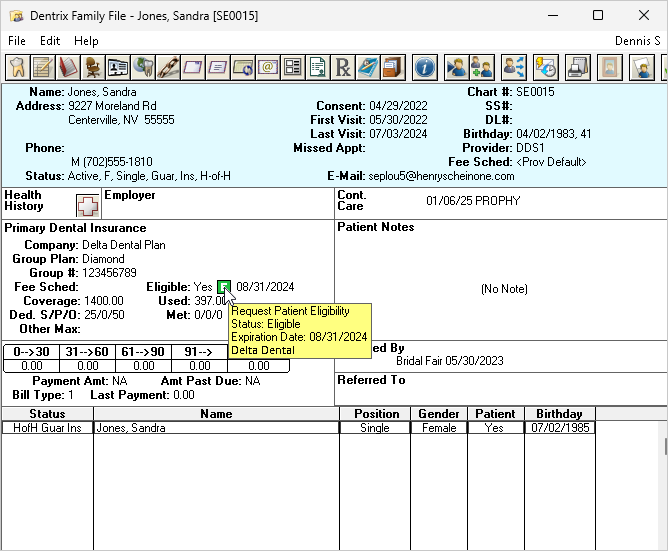
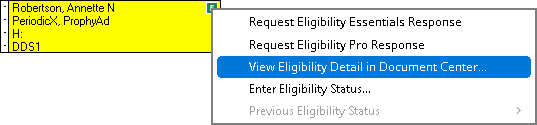
To view the complete eligibility detail that was returned with this eligibility check, click the "E" and then click View Eligibility Detail in Document Center.
This opens a document containing the patient's eligibility detail received from the insurance carrier. Dentrix saves eligibility details to the Document Center. The document is presented in a standardized layout, formatted to improve readability.
The main purpose of these requests is, of course, to report back whether the patient is eligible or not eligible. Every request will leave a "paper trail" by adding a document to the patient's Document Center. In the upper-left corner of the document, you'll clearly see the result of the eligibility check.
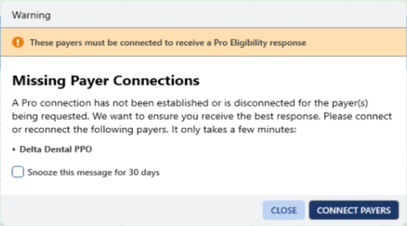
If Dentrix discovers an insurance plan on the schedule that has missing or expired credentials, you will be prompted to open the Payer Connection Portal and enter or update your username and password. Remember, if you do not enter or update the payor connection, Dentrix cannot retrieve a pro response. Dentrix will still attempt to determine eligibility, but the information returned will be at the essentials level.
Eligibility Essentials submits the patient's information using the industry standard electronic data Interchange (EDI). No special credentials are necessary to make these requests.
Many carriers will send additional information with this check. Some carriers are generous with the information shared over an EDI request, but many are not. The amount and timeliness of the information can vary greatly from payer to payer.
In contrast, payers usually keep the information on their portals complete and up-to-date.
Eligibility Pro will check both sources. It will make a standard EDI request AND use your office's login credentials to check the insurance payer's web portal. Depending on what the payer includes on their portal, Eligibility Pro can often get details such as patient history, frequency limitations, and procedure-level coverage percentages.
When you view eligibility responses, look at the Response Type on upper-left of the first page.
If you're using not seeing "Eligibility Pro" results, double-check the credentials that you provided for this payer within the Payer Connection Portal.
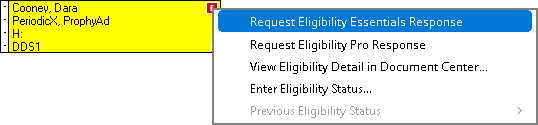
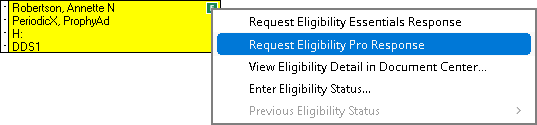
At times, you may need to submit an eligibility verification request manually. For example, this might be necessary if the automatic check returned an error, and you have since corrected the patient or insurance information.
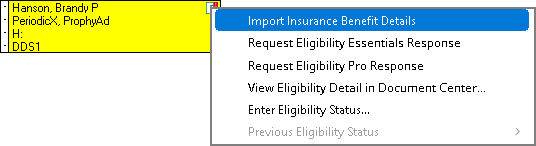
To resubmit another eligibility request manually, click the "E" on the patient's appointment and select either Request Eligibility Essentials Response or Request Eligibility Pro Response.
Notes:
Eligibility Essentials can help you update insurance benefits and coverage information. You'll save time and avoid the potential errors caused by manual data entry.
Watch this video to become familiar with importing eligibility benefits (Duration 3:12).
To begin importing, click the eligibility icon.
![]()
From the menu, select Import Insurance Benefit Details.
By clicking the tabs at the left of the Eligibility Benefit Details window, you can review the eligibility information.
The opening screen displays the patient details. These details come directly from Dentrix. This information is not editable and does not get imported.
When you receive eligibility results for a patient, the payer often includes coverage information for more than one type of plan under their umbrella (examples: In-Network, Out of Network, PPO, etc.). Use the Choose Network Plan menu to select this patient's plan type and ensure you compare and import the correct coverage.
The Insurance Plan tab will display information about the plan.
Click Deductibles and Maximums to see proposed updates to the patient's benefits table. This information will often include the deductibles met and the benefits used to date.
Click Coverages to see the proposed update to the plan's coverage table. Each category can be expanded for additional detail. Importing coverage information will affect all the patients tied to this insurance plan.
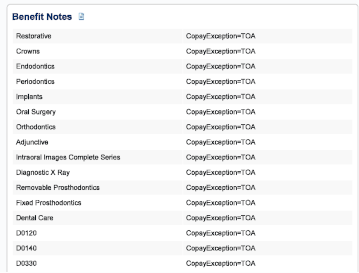
The Exceptions and Limitations section shows restrictions such as age, frequency, waiting period and exception or benefit notes for the plan.
After reviewing each piece of information, click Import.The window that opens will offer to import everything, but you can remove the selection on individual items to skip bringing that information into Dentrix.
To finalize the import, click Yes.
When coverage, deductibles and maximums, or exceptions are imported as Out-of-Network benefits, Dentrix will automatically copy the same information to the corresponding in-network areas. This will allow treatment plan estimates to utilize the information.
When "TOA" appears on your benefits breakdown, it indicates that the insurance plan has a "Table of Allowance." In this case, the benefits offered fall within a range of numbers, and an exact amount cannot be included in the eligibility result. You will need to refer to the table of allowance provided by the carrier to understand the coverage information.
An Eligibility Pro Usage Report details how many pro level responses your office receives each month.
1. Launch the Payor Connection Portal
Open the Dentrix Office Manager and click Maintenance > Reference > Payer Connection Portal
2. Select the Eligibility Pro Usage Report tab.
For practices subscribed to an Eligibility Pro plan, the following columns are available:
Limit Status - indicates if your office is below, closely approaching, or exceeding the monthly allotment.
Usage - indicates the number of received Pro responses compared to the amount allotted each month.
Overage - indicates how many requests have been made exceeding the monthly allotment. These are billed as a separate charge above the monthly subscription price.
For practices subscribed to a Eligibility Essentials with Pro On Demand plan, the usage column will display the total pro requests made in that calendar month. The Limit Status and Overage columns will appear blank.
Responses included are only those that were requested as AND successfully returned as a Pro level response.
Responses that were returned at the Essentials level (EDI) do not count as Pro responses and will not be counted on the report.
If a Pro response was requested, but failed with any error, it is not reported or counted.
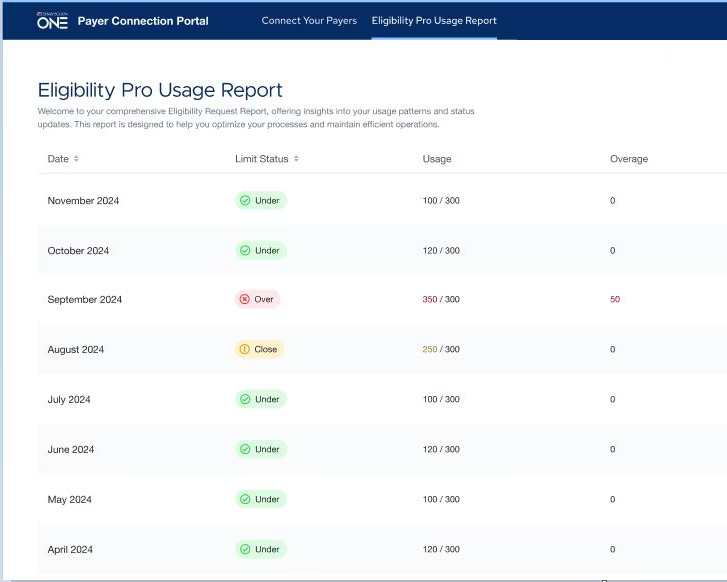
Example report of an office subscribed to an Eligibility Pro package with a monthly allotment of 300 Pro responses per month.
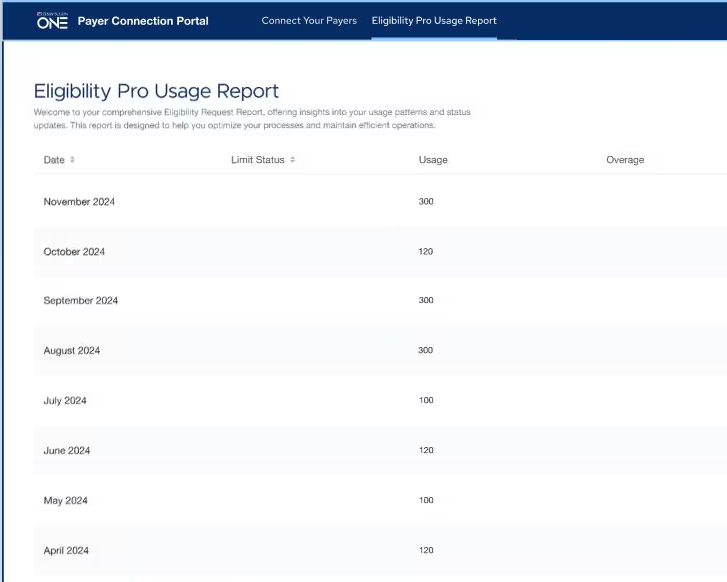
Example report of an office subscribed to an Eligibility Essentials with Pro On Demand, which does not include a monthly allotment of Pro responses.
Read the Eligibility Essentials and Pro FAQ.
View eligibility instructions in the Dentrix Help.
Use the Payer Search Tool to identify electronic connectivity for the Payers/Insurance companies you work with.