

Before you can use Dentrix Eligibility Pro and obtain enhanced eligibility responses, you must set up your insurance website credentials through the Payer Connection Portal. By doing so, you can obtain the benefits and coverage data you need without having to visit each insurance website separately.
Notes:
· When you submit an eligibility request to an insurance carrier that supports web crawler, your credentials are used to access the carrier's website from which you can collect benefit and coverage details.
· Through the Payer Connection Portal , you can also maintain your credentials as they expire over time.
To set up the Payer Connection Portal
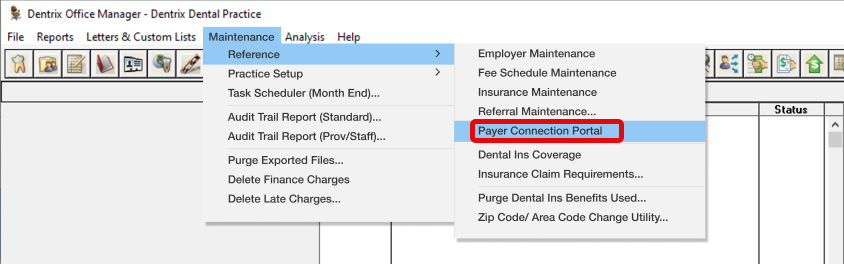
1. In the Office Manager, click Maintenance, point to Reference, and then click Payer Connection Portal.
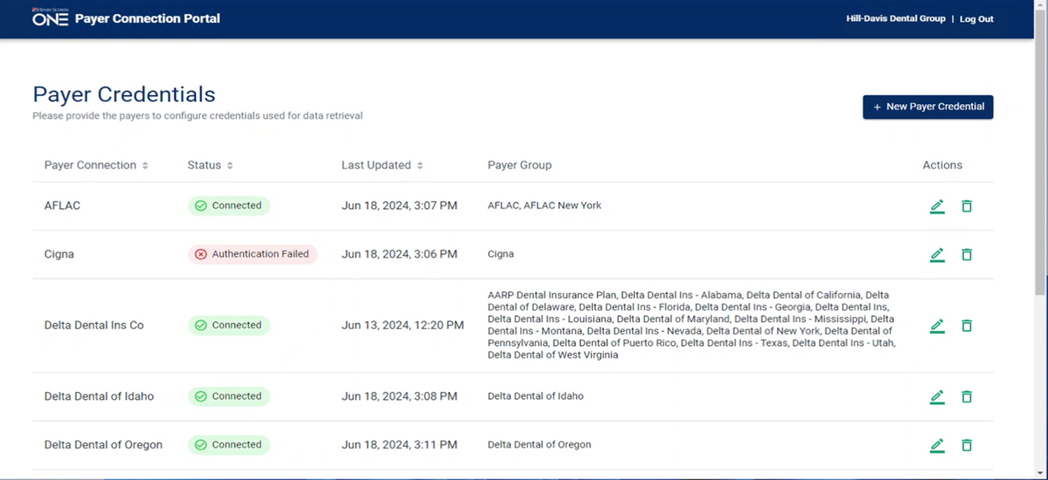
You are logged in automatically to the Dentrix Payer Connection Portal, and your credentials are passed to tuuthfairy and stored. The Payer Connection Portal appears.
2. From the Payer Connection Portal, click New Payer Credential.
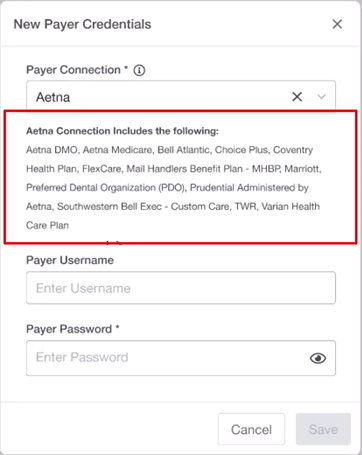
A message appears explaining that several payers are included under the umbrella of the payer connection you selected.
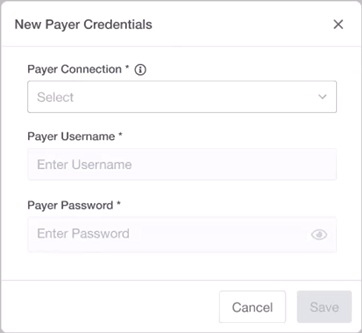
3. From the Payer Connection list, select the desired payer.
A message appears explaining that several payers are included under the umbrella of the payer connection you selected.
4. Enter the Payer Username and Payer Password that your office uses to log in to the selected website, and then click Save.
If the payer requires two-factor authentication, the following notice appears.
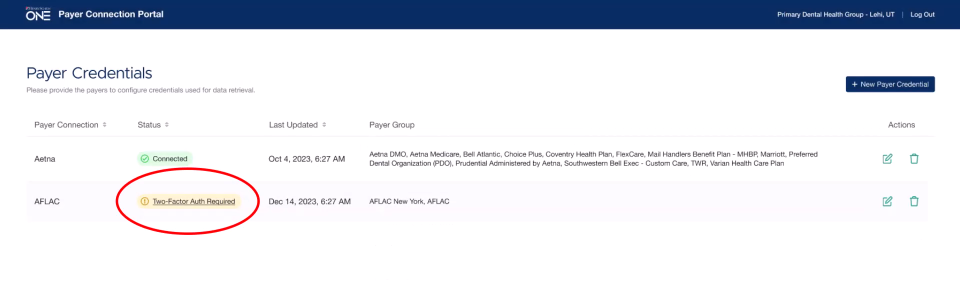
5. Once you receive the required authentication code, click Two-Factor Auth Required, enter the code, and then click Verify.
Dentrix completes the connection to the payer, and the Payer Connection Portal appears reporting your connection status with the payer websites.
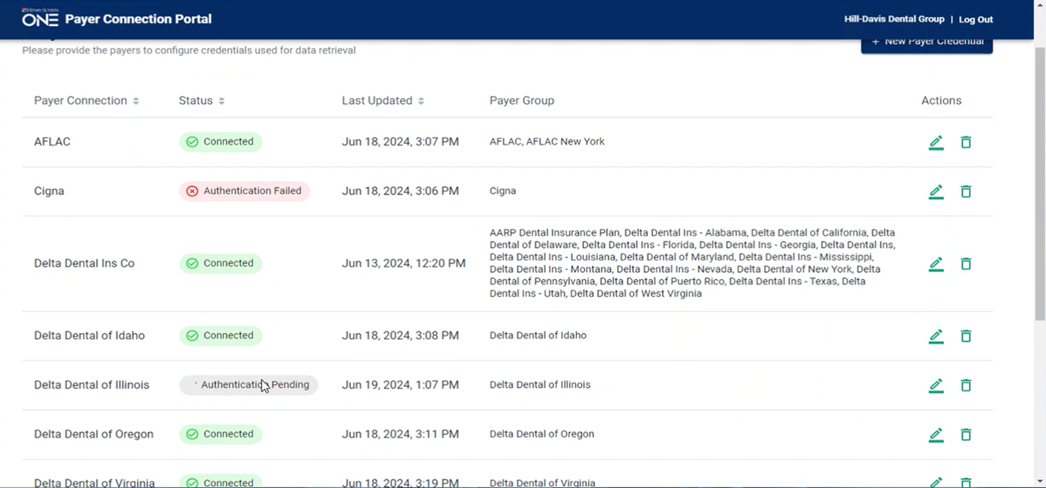
6. If an authentication fails, click the Edit icon to the right of the payer list and check the credentials you entered in the Edit Payer Credentials dialog box.
If an Eligibility Pro request is sent to a payer (either in a batch or on-demand), and that payer has a web connection, and the requesting office’s web credentials are established, then tuuthfairy queries the web first to try to get the eligibility and benefits information from that web source (as it’s the most complete).
Note: If the payer supports an EDI connection, tuuthfairy will access both web and EDI sources and merge the data to provide the most complete response possible as follows:
· If tuuthfairy can access data from both connections, the “source” in the PDF file will appear as “Web & EDI.”
· If tuuthfairy can access data from only the web, the “source” in the PDF file will appear as “Web.”
· If tuuthfairy is unable to access data from the web, it will try the EDI connection (if the payer has one). If the EDI is successful, the “source” in the PDF file will appear as “EDI.”
Notes:
· Even though an Eligibility Pro response is requested, the software still returns EDI if it can’t get a web response, so your office still receives a response. (You are only charged for Eligibility Pro responses if they are returned with a source of “Web” or “Web+EDI.”
· Some payers (such as BCBSTX, Delta SD, Delta OR) do not support an EDI connection and are web only. In this case, if a web request fails, then EDI will return “Payer Not Participating.” Our payer list will indicate what payers support which type of response.