

If you submit secondary insurance claims through DentalXChange, you must complete the Claim Adjustment Segment (CAS)/Coordination of Benefits (COB) portion for secondary insurance claims.
If you submit secondary insurance claims through DentalXChange without completing the CAS/COB portion for the primary claim, they may be rejected, and you will receive a message similar to one of the following: "COB claim balancing failed total charge amount," "Claim amount does not equal sum of paid amount and all adjustment amounts," or "Other Carrier Claim Out of Balance."
Receipt of one of these rejection messages results from the absence of, or invalid information in, the Claim Adjustment Segment, which represents primary insurance claim adjustments. Adjustment information helps the secondary provider balance the remittance information. Adjustment amounts should fully explain the difference between the submitted charges and the amount paid by the primary insurance carrier. Claims submitters must use the Claim Adjustment Segment to report the primary carrier's claim level adjustments that caused the amount paid to differ from the amount originally charged.
To complete the Claim Adjustment Segment of a primary insurance claim
1. With a patient selected in the Ledger,double-click the primary insurance claim.
The Primary Dental Insurance Claim window appears.
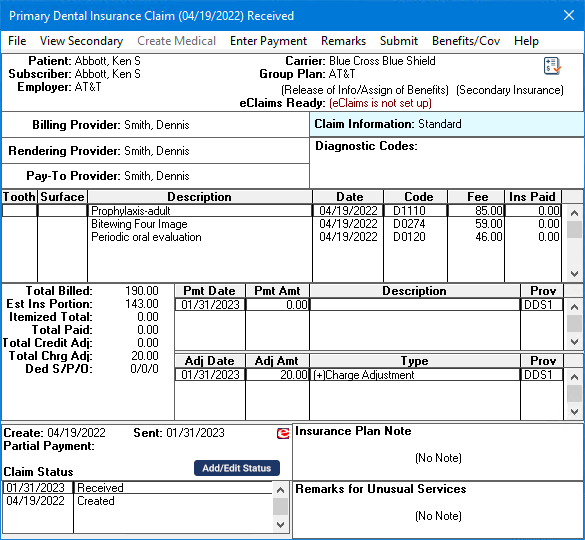
2. Click View Secondary, and then double-click the Claim Information box.
The Insurance Claim Information dialog box appears.
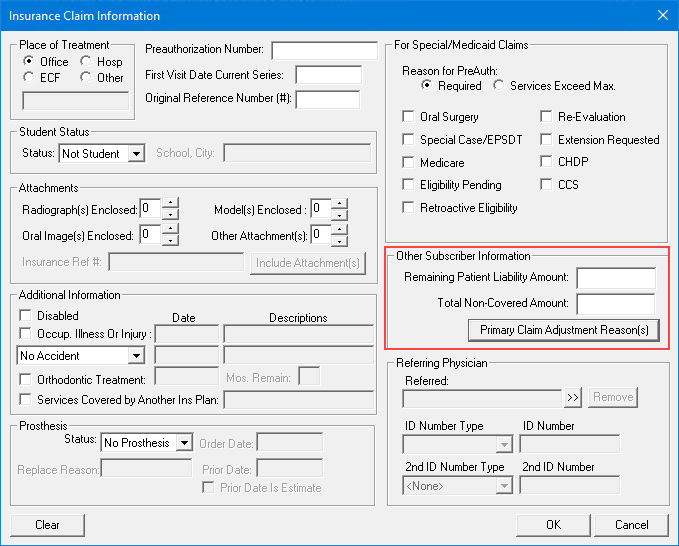
3. Under Other Subscriber Information, click Primary Claim Adjustment Reason((s).
The Primary Claim Adjustment Reason(s) dialog box appears.
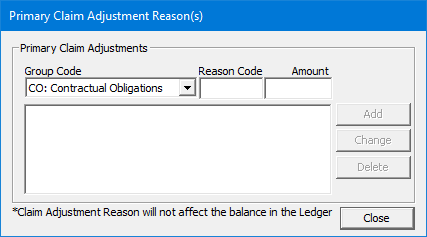
Note: All of the information that the codes represent should appear in the Primary Insurance EOB. However, if the EOB is a paper remittance, the codes may not appear, and you must manually enter the proper codes in their proper context. See step 4.
4. Complete the following information about the adjustment:
· Group Codes –
· PR – Patient Responsibility – Is the adjusted amount in the segment the patient's responsibility?
· CO – Contractual Obligation – Is the adjusted amount not the patient's responsibility due to a contractual obligation between the provider and the payer or a regulatory requirement? For example, a participating provider agreement might be considered a contractual agreement.
· PI – Payer Initiated – In the payer's opinion, is the amount in this segment not the patient's responsibility without a supporting contract between the provider and the payer?
· OA – Other Adjustment – Use if no other category is appropriate.
· CR – Correction and Reversals – Is the claim a reversal of a previously reported claim or claim payment?
· Reason Codes – The reason code appears on the ERA/EOB/EEOB that is returned from the payer after you first submit the claim. If necessary, you can use that reason code to resubmit the primary and the secondary claim.
· Reason Codes 01-03 – Always use with PR - Patient Responsibility.
Note: Always enter Reason Codes 01-09 as double digits, not 1-9.
· Reason Code 18 – Use only with OA - Other Adjustment unless the state workers' compensation regulations require CO - Contractual Obligation.
· Reason Code 23 – Use only with QA - Other Adjustment.
· Reason Code 45 – Use only with PR - Patient Responsibility or CO - Contractual Obligation depending on liability.
· Reason Code 85 – Use only with PR - Patient Responsibility.
· Reason Code 133 – Use only with QA - Other Adjustment.
· Reason Code 136 – Use only with QA - Other Adjustment.
· Reason Code 201 – Use only with PR - Patient Responsibility.
· Reason Code 209 – Use only with QA - Other Adjustment.
· Reason Code 229 – Use only with PR - Patient Responsibility.
· Reason Code 238 – Use only with PR - Patient Responsibility.
· Reason Code 249 – Use only with CO - Contractual Obligation.
· Reason Code 255 – Use only with QA - Other Adjustment.
· Reason Code 257 – Use only with QA - Other Adjustment.
· Reason Code P3 – Use only with PR - Patient Responsibility.
· Reason Code P11 – Use only with QA - Other Adjustment.
· Reason Code P16 – Use only with CO - Contractual Obligation or QA - Other Adjustment.
· Reason Code W5 – Use only with CO - Contractual Obligation or QA - Other Adjustment.
· Amount – Amount of the adjustment.
5. Click Close.
6. In the Insurance Claim Information dialog box, in the Remaining Patient Liability Amount box, enter the patient portion from the ERA/EOB (primary claim amount minus the primary claim payment amount minus adjustments).
Note: The amount paid by the primary insurance carrier plus all the adjustment amounts (the CAS segment) must equal the total amount of the claim being sent to the secondary insurance carrier. (In other words, if you subtract the amount paid by the primary insurance carrier, the remaining patient liability, and any claim adjustment amount(s) from the total charged amount, the balance should be zero (0), as shown in the following example:
Total amount charged: $100
Minus primary claim payment: -$70
Minus patient portion: -$20
Minus Claim adjustments: -$10
This balance must be $0: $0
7. Click OK.